Can I get rabies if a dog scratches me
Health Risks of a Dog Scratch
Dogs are among the most popular animal companions. In fact, its estimated that dogs live in about
Still, as with having any other pet, its important to be aware of the variety of diseases and health risks that may be transmitted from your canine companion. Some of these health risks may be derived from dog scratches that arise from playing, feeding, and coming into contact with an unknown animal.
Not all dog scratches are serious, but its important to be on the lookout for possible signs of infection, and call a doctor to rule out more serious health consequences.
Read on to learn about possible health risks from dog scratches and how to treat and prevent them.
Daily interactions with your dog including playtime can sometimes result in scratches. These might occur from your dogs nails when they step on you or jump up on you, as well as accidentally scratching you with their teeth while playing fetch or during feedings.
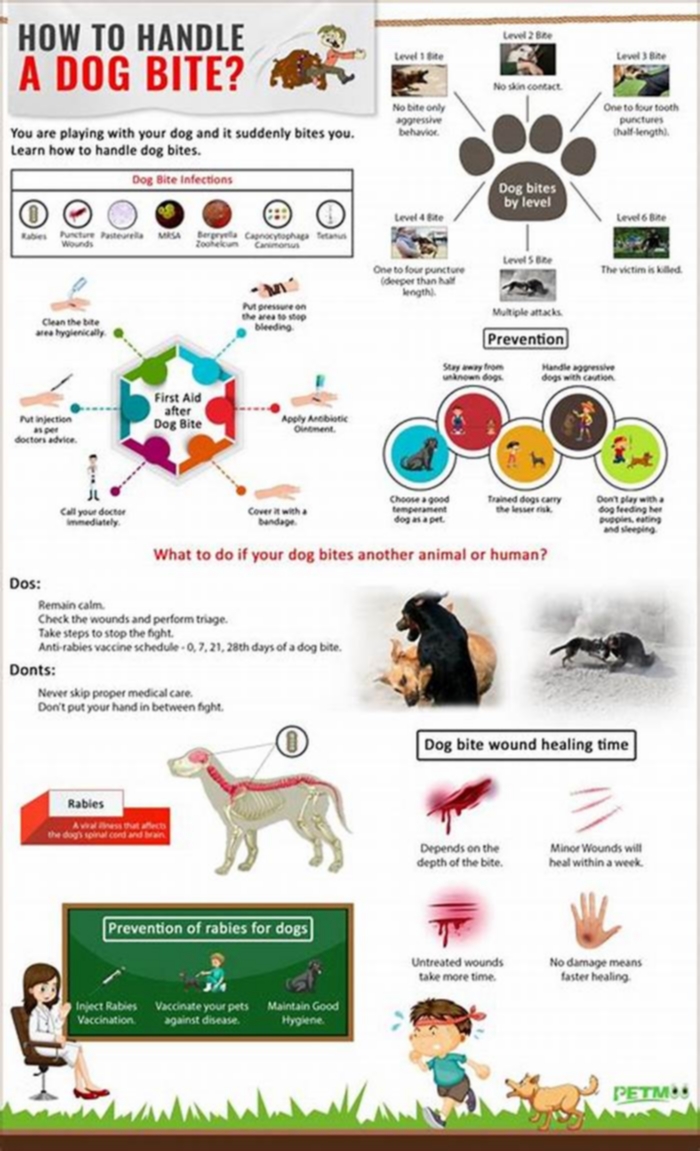
When you get scratched by a dog, you may notice red marks on your skin. These may temporarily become painful and swollen and, in more severe cases, lead to more serious health risks. Possibilities may include:
- excessive bleeding
- infections, such as Capnocytophaga bacteria
- tetanus, which is caused by Clostridium tetani bacteria
- rabies, a serious viral infection
- sepsis, a life-threatening emergency caused by the spread of an infection to vital organs
Any dog scratch including those that seem mild and harmless ought to be treated immediately to prevent infection and other health complications. Consider the following steps:
- First, wash (but dont scrub) the dog scratch wound with warm water and soap. Rinse for at least 5 minutes. Pat dry with a clean towel.
- If the dog scratch is bleeding, apply pressure to the area with a clean gauze pad.
- Apply an over-the-counter (OTC) antibiotic cream or ointment.
- Cover the wound with a sterile bandage.
Some dogs carry a bacteria in their mouths called Capnocytophaga. While these bacteria
Capnocytophaga infections can progress quickly, even becoming life-threatening. Possible symptoms
- swelling
- redness and blisters
- pus from the bite
- fever
- headache
- muscle or joint aches
- abdominal pain
- diarrhea
- vomiting
Call or visit a doctor if youre experiencing any signs of infection post-dog scratch. Its also a good idea to seek medical attention any time youve been scratched by a dog especially if the dog isnt your own.
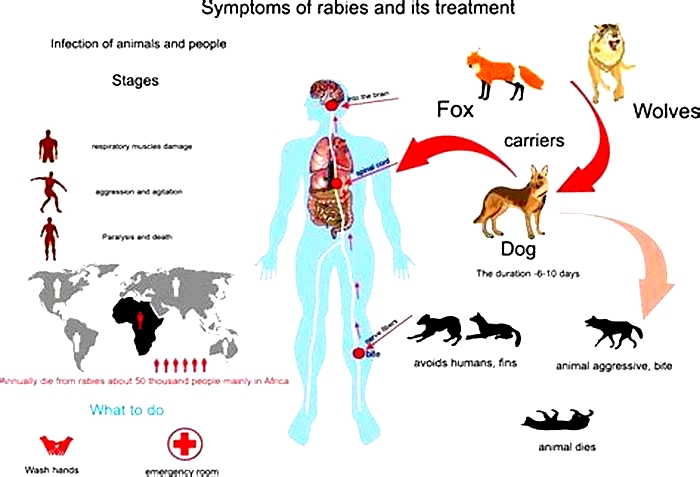
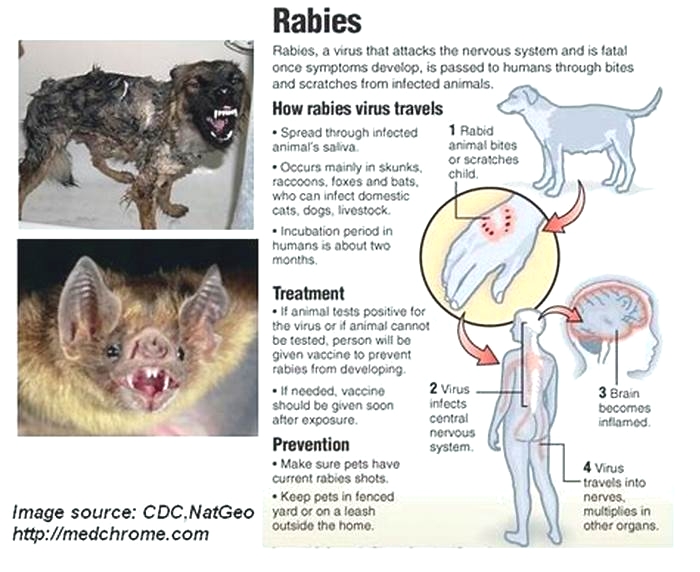
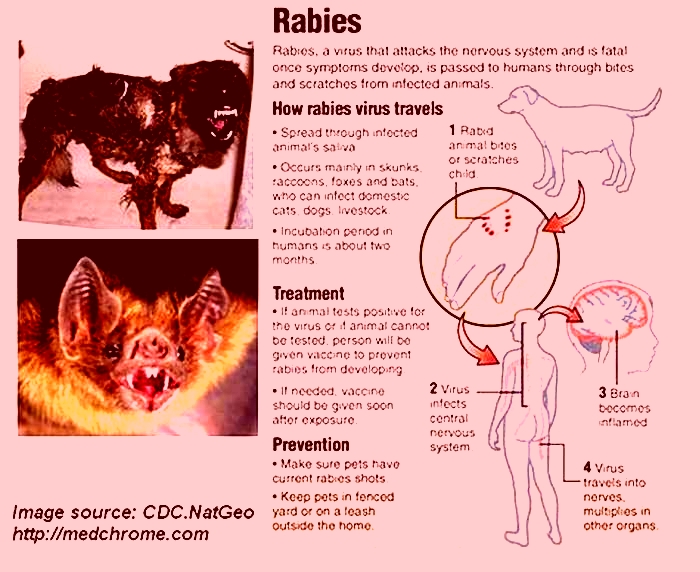
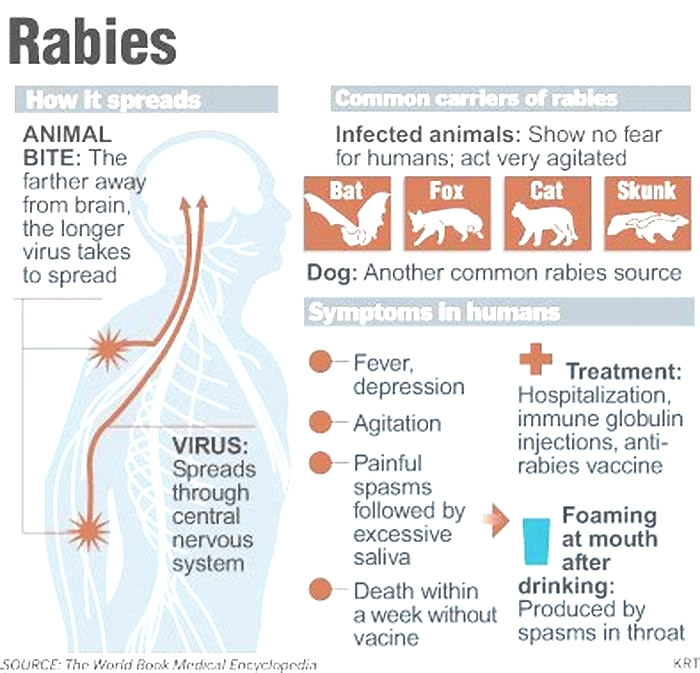
Rabies is a type of viral infection that can occur when bitten by an animal thats infected. This is a serious infection that can be fatal in both animals and humans, due to the viruss attack on the nervous system.
While animal-to-animal transmission is possible, its not as common for humans to be infected by household pets in the United States. Part of this reduced risk is attributed to rabies vaccines in domesticated animals.
Still, rabies ought to be considered in the case of a serious wound from a dog, particularly if its a stray dog or one who hasnt been vaccinated against rabies. The virus may be transmitted through an infected dogs saliva from biting or accidental scratching.
How a dog with rabies may behave
A dog who is infected with rabies may have
- behavioral changes
- reduced appetite
- voice changes/changes to their barks
- panting
- anxiety and restlessness
- attempted attacks on people and other animals
- paralysis
What to do if you suspect youve been bitted by a dog with rabies
If youve been bitten or scratched by a dog with an unknown rabies vaccination status, call a doctor. They may recommend treatment with rabies vaccines as well as antibodies.
Humans (with the exception of veterinarians and other professionals who handle animals) dont typically get the rabies vaccine unless theyve been exposed to the virus from an infected animal.
Symptoms of a rabies infection
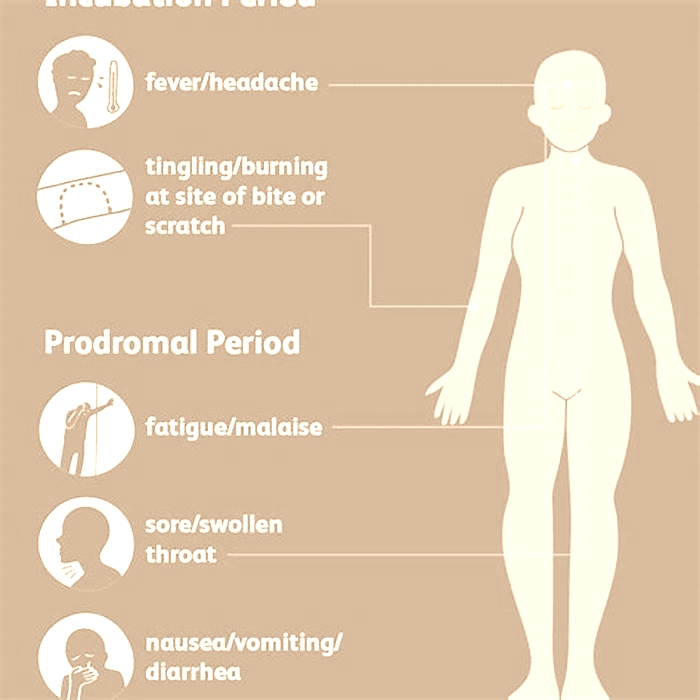
Symptoms of rabies are slow to develop,
Possible signs of rabies in humans may include:
- fatigue
- fever
- headache
- weakness
- anxiety
- hallucinations, and other neurological changes
While its not always possible to avoid all cases of dog scratches, you may help minimize your risk of getting sick by:
- washing your hands after playing with and feeding your dog
- carefully washing scratches that do occur
- bandaging dog scratches and any subsequent open wounds
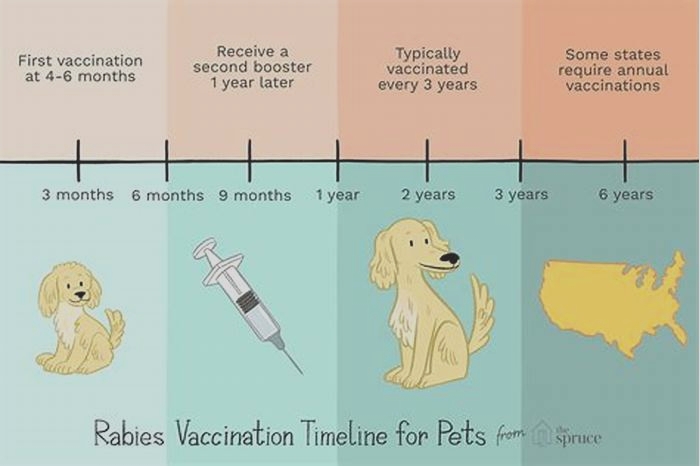
- keeping your dog up-to-date on their vaccines
- avoiding contact with other dogs that may be feral or unvaccinated
- walking your dog on a leash to prevent exposure to wild animals
- asking your doctor if youre up to date on your vaccines
Also, if you have your own dog, you may help reduce the risk of scratches from toenails and bites by training your dog not to jump up on you, and to use their mouths softly during playtime and feedings.
Getting scratched by your dog can happen, especially during feeding and playtime. While you can train your dog to be more gentle, occasional scratches are still inevitable. Your risk may also be greater when coming into contact with a wild dog, or a domesticated one whos not your own.
Washing a dog scratch wound is critical in preventing infections. Depending on the severity of the wound, you may consider calling your doctor regarding next steps.
Seek medical care if youre injured by a dog who isnt yours, if youve been bitten, are bleeding excessively, or are experiencing flu-like symptoms.
Is it possible to contract rabies from a dog scratch?
Introduction: The Risk of Rabies from a Dog Scratch
Dogs are among the most popular pets worldwide, with millions of households owning at least one. However, owning a dog comes with certain risks, especially if the dog is not vaccinated against rabies. Rabies is a fatal viral disease that affects both humans and animals and is transmitted through the saliva of infected animals. Although rare, rabies can be contracted from a dog scratch, making it crucial to understand the risk factors and preventive measures.
Understanding Rabies: Causes and Symptoms
Rabies is caused by a virus that attacks the nervous system of the infected animal or human. The virus is transmitted through the saliva of infected animals, usually through a bite. The symptoms of rabies include fever, headache, muscle weakness, seizures, and eventually, paralysis and death. Once the symptoms appear, there is no cure for rabies, making it essential to seek medical help immediately after exposure.
How Can Dogs Contract Rabies?
Dogs can contract rabies through contact with infected animals, such as bats, raccoons, and skunks. The virus is usually transmitted through bites, but scratches and licks on open wounds or mucous membranes can also spread the virus. Dogs that are not vaccinated against rabies are at a higher risk of contracting the disease. In some cases, dogs can spread the virus to humans through bites or scratches, making it essential to take preventive measures to avoid exposure.
Risk Factors for Contracting Rabies from a Dog Scratch
The risk of contracting rabies from a dog scratch depends on several factors, such as the severity of the scratch, the location of the wound, and the vaccination status of the dog. Dogs that are not vaccinated against rabies pose a higher risk of transmitting the virus to humans. Moreover, scratches on the face, neck, or hands are more likely to transmit the virus than scratches on other body parts. It is also crucial to consider the behavior of the dog, as aggressive or erratic behavior may indicate the presence of rabies.
Transmission of Rabies through Saliva
Rabies is primarily transmitted through the saliva of infected animals, usually through bites. However, the virus can also be transmitted through scratches or licks on open wounds or mucous membranes, such as the eyes or mouth. Once the virus enters the body, it travels to the nervous system, where it can cause severe damage and ultimately lead to death. It is crucial to seek immediate medical attention after exposure to reduce the risk of contracting rabies.
What to Do If You Get Scratched by a Dog
If you get scratched by a dog, it is essential to clean the wound thoroughly with soap and water. If the scratch is severe, seek medical attention immediately. It is also crucial to ask the owner of the dog about the vaccination status of the dog and its behavior. If the dog is not vaccinated or shows signs of rabies, contact your healthcare provider immediately to assess your risk of rabies exposure.
Diagnosis of Rabies in Dogs
Diagnosing rabies in dogs involves testing brain tissue samples for the presence of the virus. The testing is usually done after the dog has died or been euthanized. However, in some cases, a live animal test can be performed, which involves taking a sample of saliva or spinal fluid. It is crucial to report any suspected cases of rabies in dogs to the local health department to prevent the spread of the virus.
Treatment for Rabies in Humans
There is no cure for rabies once symptoms appear, making it crucial to seek medical attention immediately after exposure. Treatment for rabies involves a series of injections to prevent the virus from spreading in the body. The treatment is most effective when started early, before symptoms appear. It is crucial to follow the recommended treatment plan and attend all scheduled appointments to reduce the risk of contracting rabies.
Prevention of Rabies: Vaccination and Safety Measures
Preventing rabies involves vaccination of dogs and taking preventive measures around animals. Dogs should be vaccinated against rabies regularly, as recommended by the veterinarian. It is also crucial to avoid contact with stray or wild animals, especially those that show signs of rabies. If you have a dog, keep it on a leash and monitor its behavior around other animals and humans. It is also crucial to teach children to avoid approaching unfamiliar dogs.
Laws and Regulations on Rabies in Dogs
Many countries and states have laws and regulations on rabies in dogs, including mandatory vaccination and quarantine requirements. It is crucial to follow these laws and regulations to prevent the spread of rabies and protect public health. Failure to comply with these laws can result in fines or legal action.
Conclusion: Staying Safe around Dogs
Rabies is a fatal viral disease that can be contracted from a dog scratch. Understanding the risk factors and preventive measures is crucial in staying safe around dogs. Vaccination of dogs and taking preventive measures around animals can help prevent the spread of rabies. It is essential to seek medical attention immediately after exposure to reduce the risk of contracting rabies.
Resources for Rabies Information and Assistance
For more information on rabies, contact your local health department or veterinarian. The World Health Organization and Centers for Disease Control and Prevention also provide information on rabies prevention and treatment. In case of exposure, contact your healthcare provider or local health department for assistance.
Travel Health Journal
Rabies is one of the most deadly infections known to humans. Its also 100% preventable.
Rabies has been recognized in humans since 2000 B.C. Despite its long history, it continues to cause approximately 59,000 deaths a year, mostly among children. The virus that causes Rabies is present around the world (with the exception of Antarctica) and all mammals are susceptible to infection.
This World Rabies Day, find out the truth behind 5 common misconceptions so you can stay informed and help others stay safe. We take a look at why Rabies is still a concern, how travellers are at risk, and what you can do to be prepared.
1. Rabies is only transmitted by animal bites: FALSE.
Rabies is transmitted through contact with the saliva of an infected animal. Bites are the most common mode of Rabies transmission but the virus can be transmitted when saliva enters any open wound or mucus membrane (such as the mouth, nose, or eye). As a result, licks or scratches from rabid animals can also transmit the virus.
Canines, particularly dogs, are the most common source of Rabies transmission worldwide because they bite readily and often have contact with humans and other animals. Canine Rabies a specific type of Rabies that is spread among dogs, foxes, coyotes, wolves, and other canines is still endemic (meaning it is regularly found) in parts of Africa, Asia, and Central and South America. In these regions, there are significant challenges to reducing Rabies in canines such as low vaccination rates in dogs, limited and costly veterinary services, lack of public awareness, and uncontrolled dog populations.
Most Rabies deaths occur in Africa and Asia and are due to bites, scratches, or licks from dogs. In Europe, Canada, and the United States, human Rabies cases are rare because most dogs are vaccinated against it. In these regions, Rabies is most often reported in wild animals such as raccoons, skunks, and foxes.
2. A bite from an animal will be obvious: FALSE.
In Canada and the United States, most human Rabies infections are associated with bats. Due to their small size, bat bites or scratches may not be noticeable or leave no obvious puncture wounds.
Bat rabies occurs in every country (with the exception of New Zealand and Antarctica). Bats are a high risk vector for Rabies transmission because bite wounds or scratches can go undetected and therefore untreated. In some circumstances, the victim may not even know they had contact with a bat bats become most active at night and may bite or scratch a person while they sleep. Its important to seek medical care immediately if you wake up in a room with a bat or if someone who cant report a bite (such as a child or person with a disability) has unsupervised contact with a bat.
3. Animals will clearly appear rabid and unwell: FALSE.
While most animals will demonstrate some signs of illness such as aggression or lack of balance, some may not have noticeable symptoms.
Wherever you go, its important to avoid contact with wild or feral animals. In countries with canine Rabies, avoid contact with dogs and other biting mammals (such as monkeys), particularly if they are acting strangely. Teach children not to pet, feed, or play with animals even if the animal is friendly. Encourage them to report any contact with an animal and reassure them that it is not their fault if they get bitten or scratched.
If you or your child are bitten or scratched by an animal, wash the wound thoroughly with soap and water, rinse it with antiseptic, and immediately seek medical care.
4. The symptoms of a Rabies infection will appear shortly after a bite: FALSE.
After the bite of an infected animal, Rabies symptoms may take weeks, months, or in some cases, years to appear in humans (this is known as the incubation period). The length of time before symptoms appear can vary based on where you were bitten (arm, leg, face, etc.), the type of Rabies infection (bat or canine), and if you were vaccinated against Rabies before the bite. The long incubation period of Rabies can make diagnosis and treatment difficult because patients may assume no infection occurred until symptoms develop at which point the disease becomes fatal. If you suspect you were exposed to the Rabies virus, always seek prompt medical care and vaccination.
5. You can only get vaccinated against Rabies after a bite: FALSE.
The Rabies vaccine is administered in a series of vaccines, which can be given before potential exposure as a preventive measure or after a bite from an infected animal.
Depending on whether you were vaccinated before exposure or not will determine what set of Rabies vaccines you require after a bite or a scratch:
- If you were not vaccinated against Rabies, you need a series of 4-5 vaccines and the Human Rabies Immunoglobulin (HRIG) over a period of 14 days after the bite or scratch.
- If you were vaccinated with a series of 3 pre-exposure vaccines, you have some initial protection. In the event that you are bitten or scratched, you only need 2 post-exposure vaccines. HRIG is not required. *
*These are current guidelines used in the United States and Canada. The World Health Organization recently released revised Rabies vaccination guidelines that support a condensed vaccination schedule and dosage. The new schedule is proven to provide adequate protection and reduces the cost of vaccination.
HRIG is highly delicate and expensive. It is made from the donated blood plasma of people who have been vaccinated against Rabies. After potential Rabies exposure, HRIG must be administered promptly with the first dose of the Rabies vaccine series. It provides immediate immunity until the Rabies vaccines can begin to provide long-term protection (after about 7 days). In some countries, Equine Rabies Immunoglobulin (ERIG) may be administered when HRIG is not available. ERIG is made from the plasma of horses.
HRIG is in short supply worldwide, particularly in countries that are most affected by Rabies. Rabies is classified as a Neglected Tropical Disease because the infection disproportionally affects low-income populations in developing regions where medical services are limited (particularly in rural areas) and necessary post-exposure Rabies vaccines are often unavailable or in short supply.
Should you get vaccinated against Rabies?
For travellers, the risk of Rabies transmission will depend on where you are going, how long you are travelling for, and the type of activities you participate in. Consider getting the pre-exposure series before departure if youre at increased risk of having contact with infected animals, such as if you are:
- Planning an extended stay or on work assignments in remote and rural areas, particularly in Rabies endemic regions (Africa, Asia, and Central and South America).
- Working directly with animals.
- Going to areas with limited medical care and limited access to post-exposure Rabies vaccines.
- Participating in high risk activities such as hiking, camping, running, cycling, or exploring caves in endemic regions.
The benefit of the pre-exposure series is that after potential exposure to the Rabies virus, only 2 post-exposure vaccines are required and HRIG is not needed. This greatly simplifies post-exposure care, as unvaccinated travellers may need to be emergency evacuated or travel to another country to find HRIG and adequate post-exposure medical care. The need to seek vaccination promptly and the high cost of HRIG can easily derail a trip and lead to unexpected expenses.
To the average traveller, the chances of encountering a rabid animal may be low but being aware of the risks and the difficulty of accessing emergency care are an important component of responsible travel.
Photo by Canva.
Article by Claire Westmacott.