Can a small bite cause rabies
Can a small dog bite cause rabies?
There is no one answer to the question of whether a small dog can cause rabies, as the risk depends on a variety of factors. However, some people believe that it is possible for a small dog to bite someone and then contract the virus. If this happens, it is important to get the dog checked out by a professional who can look into its health and see if there is any risk of contracting rabies.
What happens if a small dog bites you?
Small dogs are not as dangerous as they may seem. In fact, they can often be quite friendly and playful. However, there are a few things that can happen if a small dog bites you. If the bite is severe, you may experience pain, swelling, and even infection. In some cases, the small dog may also have been provoked into attacking by another animal in your home.
Should I worry about a small dog bite?
Small dog bites are becoming more and more common, but many people do not worry about them. There are a few things you can do to help protect yourself from a small dog bite, but it is important not to overreact.
Do I need a rabies shot for a small dog bite?
Small dog bites are common in the United States, and many people believe that a rabies shot is required for small dogs. However, this is not always the case. Some people believe that a rabies shot does not necessary occur for small dog bites, while others believe that it may be necessary for certain types of dog bites. It ultimately depends on the circumstances and your personal opinion.
Can a small scratch from a dog cause rabies?
A small scratch from a dog can cause rabies, according to the Centers for Disease Control and Prevention. If a person is infected with rabies, they may experience fever, muscle aches, itching and red eyes. There is also a high risk of getting the virus if the animal that bit you has been infected.
What happens if a vaccinated dog bites you?
Vaccinated dogs are safer than unvaccinated dogs, but there is always a risk for a bite. If you are bitten by a vaccinated dog, the best thing to do is seek medical attention as quickly as possible.
How do you know if a dog has rabies after biting?
There is no one definitive answer to this question, as the symptoms of rabies in dogs can vary depending on the extent and location of the bite. However, if a dog has bitten someone recently, or if they have been shown to be rabid in any way, its important to get a medical check-up.
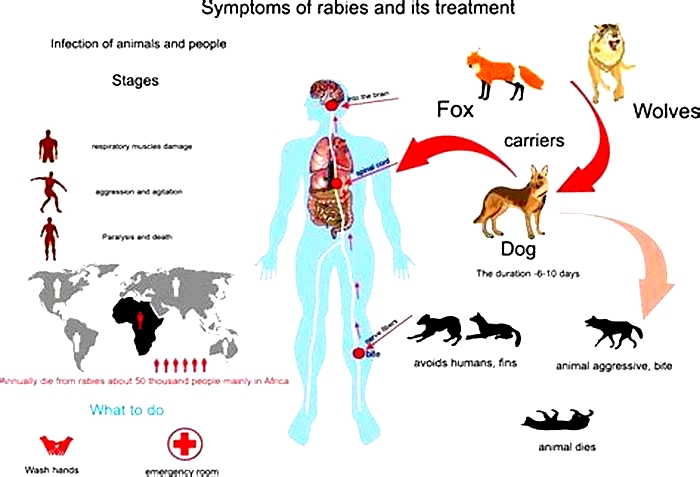
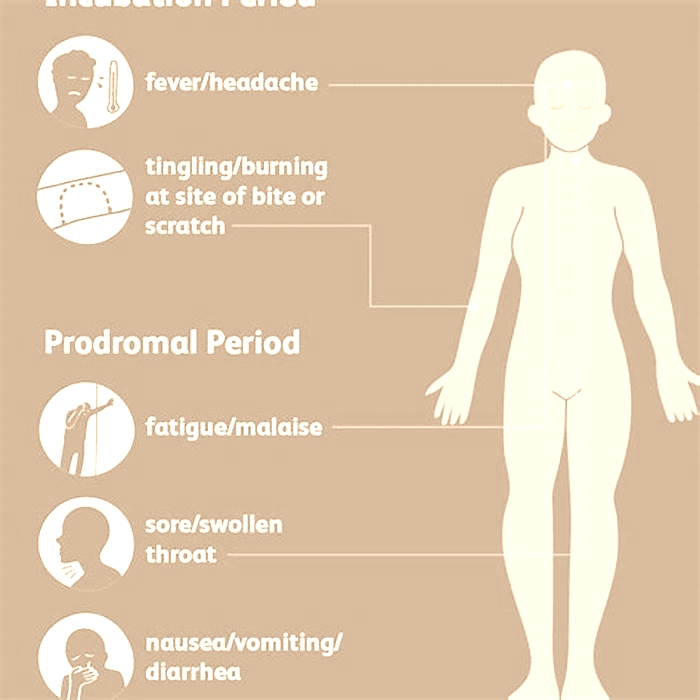
How long does it take to show signs of rabies in humans?
Rabies is a serious disease that can cause severe brain and spinal cord injuries. It is important to be aware of the signs of rabies in humans and take appropriate action if you see any of these symptoms.
Can 2 month old puppy have rabies?
There is no definitive answer when it comes to whether or not a 2-month-old puppy can have rabies. However, if the pup has recently been in close contact with an animal that has the virus, it would be best to take it to a veterinarian for diagnosis and treatment.
How soon do you need rabies shots after being bitten?
There is no definitive answer to this question, as the best time to get rabies shots depends on the individuals age and health condition. However, if you have been bitten by a rabid animal, it is important to get vaccinated against the virus as soon as possible.
Why quarantine a dog after a bite?
There are several reasons why one might want to quarantine a dog after a bite. Some dog owners believe that dogs that have been bitten may be infected with canine Jacobs syndrome, which is a condition characterized by newborn puppies displaying behavioral and physical anomalies. Another reason to quarantine dogs is when the incidence of dog bites increases because of a new trend in the community of pedestrians or cyclists who are bitten by dogs.
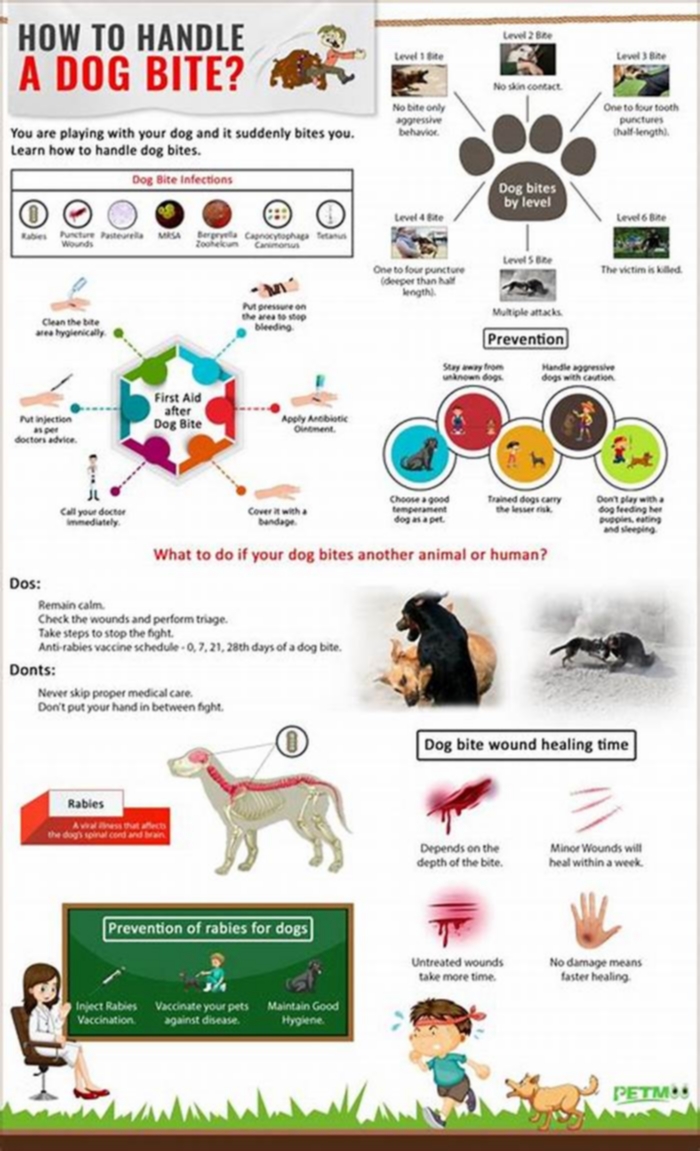
What to do after being bitten by a dog?
If you are bitten by a dog, it is important to have an emergency plan in place in case of emergencies. Here are some tips on what to do if you are bit by a dog:
1) Get medical attention as soon as possible. If you are bitten, there is a high risk that you will develop serious injuries.
Can you get rabies if the skin is not broken?
Rabies can be contracted from contact with an infected animal, but it is most commonly contracted from the saliva of a rabid animal. If the skin is not broken, rabies can be prevented by following some common precautions: washing your hands often, avoiding close contact with animals that are sick or injured, and getting vaccinated against the virus.
How do you know a dog has rabies?
The symptoms of rabies, which can be severe and include a rash, fever, paralysis, and even death, are usually seen in dogs that have been exposed to the virus. However, there is no one-size-fits-all answer to the question of whether or not a dog has rabies. In order to determine whether or not your dog has the virus, you will need to take some steps including assessing their behavior and health.
How soon after dog bite do I need tetanus?
Tetanus is a preventable disease that can happen to people of all ages. If you are bitten by a dog, the first thing you should do is call your doctor. The Centers for Disease Control and Prevention (CDC) recommends that all people get tetanus vaccines before getting any newoped, including any dog bites. However, it is important to note that not everyone who gets a dog bite needs to receive tetanus vaccines.
Conclusion
In conclusion, small dogs can sometimes bite people, and if they do, its important to get them sposed up on rabies. If you or someone you know has been bitten by a small dog, get their dog sposed up on rabies.
I am a dog lover who helps others by writing blog posts about dog-related topics. I enjoy helping people find information they may have been looking for and giving them the opportunity to interact with me in a positive way.
View all posts
Disclaimer
The post provides general informational content and is not a substitute for professional veterinary advice. The information may not be accurate, complete, or up-to-date. Readers should consult a qualified veterinarian before attempting any solutions or treatments mentioned in the post. The post disclaims any responsibility for adverse effects resulting from implementing the information without proper veterinary consultation. The well-being and safety of the pet should always be prioritized, and expert guidance from a licensed veterinarian is essential.
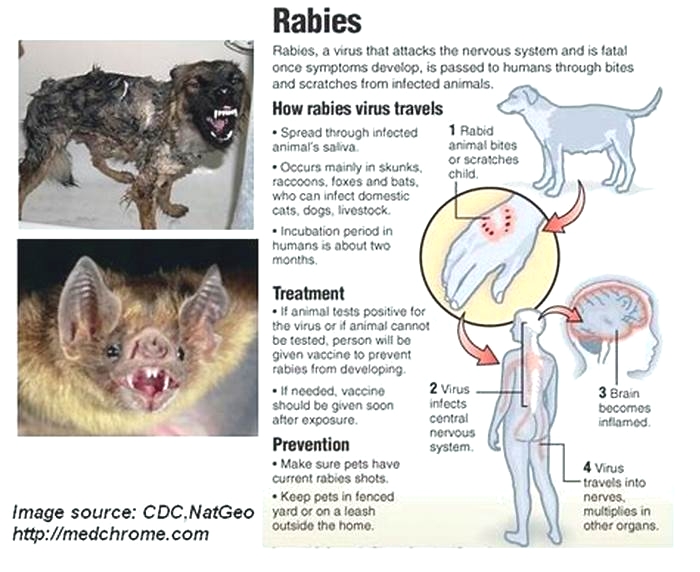
What type of exposure occurred?
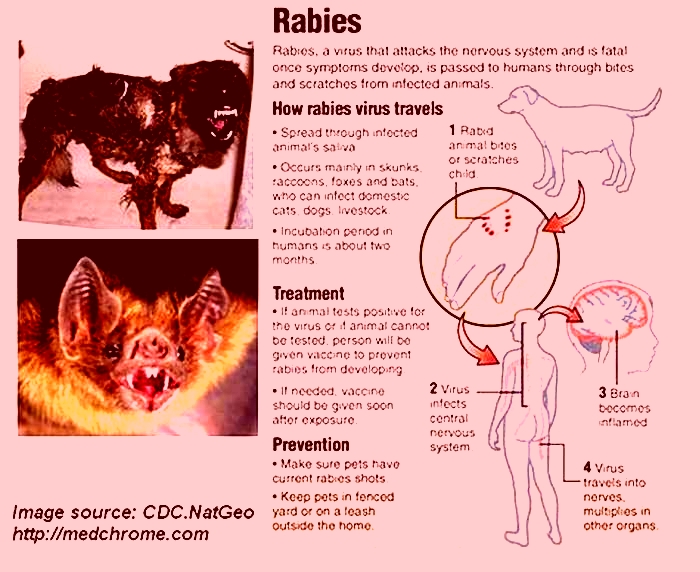
Rabies is transmitted only when the virus is introduced into a bite wound, open cuts in skin, or onto mucous membranes such as the mouth or eyes.
Other factors to consider when evaluating a potential rabies exposure include the natural occurence in the area, the biting animals history and current health status (e.g., abnormal behavior, signs of illness), and the potential for the animal to be exposed to rabies (e.g., presence of an unexplained wound or history of exposure to a rabid animal).
A currently vaccinated dog, cat, or ferret is unlikely to become infected with rabies.
When an exposure has occurred, the likelihood of rabies infection varies with the nature and extent of that exposure. Under most circumstances, two categories of exposure bite and nonbite should be considered.
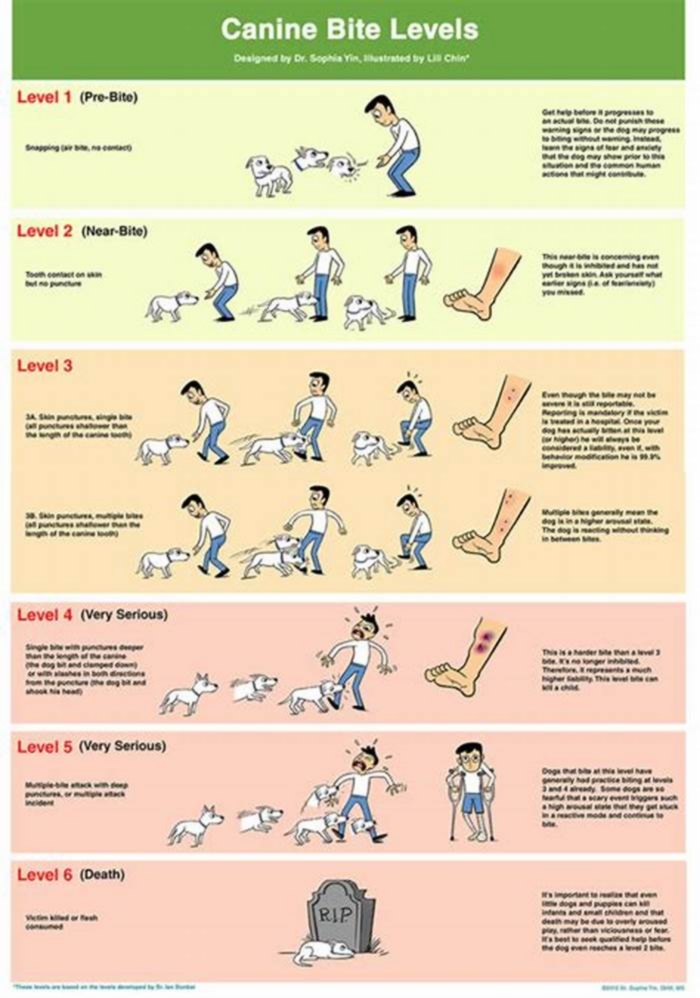
Bite
Any penetration of the skin by teeth constitutes a bite exposure. All bites, regardless of body site, represent a potential risk of rabies transmission, but that risk varies with the species of biting animal, the anatomic site of the bite, and the severity of the wound.
Bites by some animals, such as bats, can inflict minor injury and thus be difficult to detect.
Was the bite from a provoked or an unprovoked attack? Bites inflicted on a person attempting to feed or handle an apparently healthy animal should generally be regarded as provoked. If it was an unprovoked attack, thats more likely to indicate that the animal is rabid.
Nonbite
The contamination of open wounds, abrasions, mucous membranes, or theoretically, scratches (potentially contaminated with infectious material from a rabid animal) constitutes a nonbite exposure.
Nonbite exposures from terrestrial animals rarely cause rabies. However, occasional reports of rabies transmission by nonbite exposures suggest that such exposures should be evaluated for possible postexposure prophylaxis administration.
Other contact by itself, such as petting a rabid animal and contact with blood, urine, or feces of a rabid animal, does not constitute an exposure and is not an indication for postexposure vaccination.
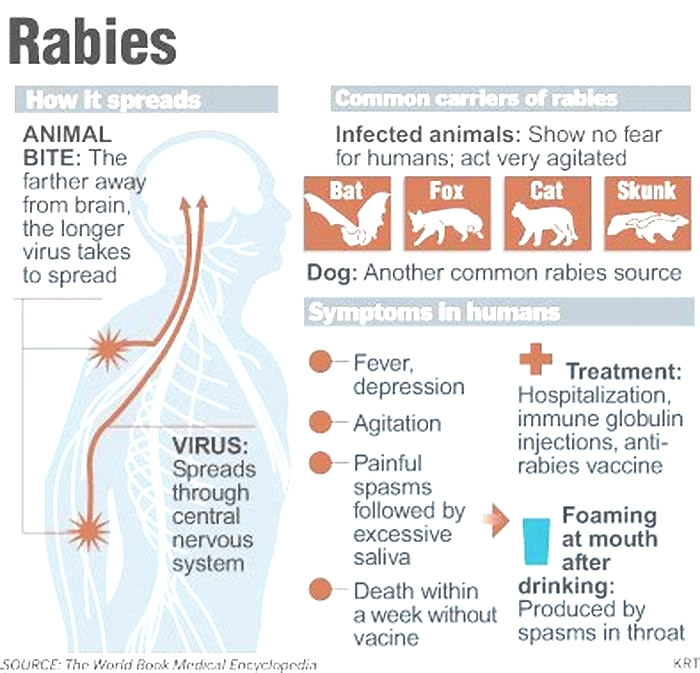
Rabies
Jason Howland:The most dangerous threat of rabies in the U.S. is flying overhead.
Gregory Poland, M.D., Vaccine Research Group Mayo Clinic:"It used to be thought, well, it's a rabid dog. But the more common way of getting rabies is from the silver-haired bat."
Jason Howland:The deadly virus is transmitted from the saliva of infected animals to humans, usually through a bite.
Dr. Poland:" The bat doesn't always bite. Sometimes the saliva will drool onto you, and you could have a minor open cut. Or sometimes a bat will lick on the skin and, again, transmit the virus that way."
Jason Howland:Dr. Poland says that's why if you wake up and find a bat in the room, you should get the rabies vaccine.
Dr. Poland:"People think, 'Well, the bat's in the house. We woke up with it, doesn't look like it bit anybody.' Doesn't matter. Rabies is such a severe disease with no cure, no treatment for it, that the safer thing to do is to give rabies vaccine."
Jason Howland:That includes an immune globulin and multidose rabies series which is not cheap. A typical series of rabies vaccines cost anywhere from three to seven thousand dollars.
For the Mayo Clinic News Network, I'm Jason Howland.
Scratches/Abrasions without Bleeding Cause Rabies: A 7 Years Rabies Death Review from Medical College Shimla, Himachal Pradesh, India
Sir,
Rabies annually causes 20,000 deaths in India and this figure has not changed for the last decade. This review was done retrospectively to analyze the reasons for deaths due to rabies, registered at Indira Gandhi Medical College Shimla since 2009. We investigated 19 deaths due to rabies in the past 7-year period. Of these, five were caused by scratches/abrasions without any bleeding and no postexposure prophylaxis (PEP) was sought. All injuries were caused either by unvaccinated pups below 3 months of age or by stray unvaccinated dogs. Four deaths were of patients who received proper wound care along with minimum 3 doses of intramuscular rabies vaccination, but rabies immunoglobulins (RIG) were not given or were not available. In eight cases, no PEP was sought as the patients were either not aware of its need or the PEP facility was far away or the PEP cost was not affordable or deceased believed that pups below 3 months of age do not carry a risk of rabies. In one case, the patient was bitten by a cat 2 years back. Majority patients belonged to rural and remote areas. Five of the deaths in our study were because of not seeking prophylaxis as abrasions/scratches without bleeding were not thought to carry a risk of rabies. In the Philippines, a rabies death review of 1839 patients demonstrates that all deaths were due to dog related injuries including bites and scratches.[1] In Iran[2] four people having scratches on their hands were infected with the saliva of rabid animals and died due to rabies, there was no history of bites. In our death review also, deaths caused by scratches/abrasions without blood amply demonstrate the ability of the rabies virus to enter nerves through dermis due to broken skin and its capacity to cause rabies. In our settings, the minimum incubation period was 22 days due to scratches on the face in front of Lt Tragus and maximum incubation period was 102 days due to a trivial scratch on right Forearm by a furious rabid dog. Rabies due to bat scratches[3] is known and hence can happen due to rabid dog/animal scratches as well. Pathogenesis studies by Kuzmin et al.[4] state that after delivery into a wound, rabies virus can infect several types of cells and replicate at inoculation site, as has been shown for skeletal muscle cells and fibroblasts. Human skin dermal layer is populated with fibroblasts that may allow the entry of the rabies virus and subsequent infection if left unattended[5] and needs further evaluation. Latest guidelines of the WHO (2014) prescribe that the type II wounds, that include minor scratches or abrasions without bleeding, need to be given only rabies vaccine whereas additional local RIG infiltration may be required.[6] The confusion of scratches with blood or without blood need to be rectified in the type II classification of the WHO bite wounds and need to be replaced by Bruises that don't involve breach of the skin surface. Breach of skin surface can easily be identified with spirit test, if there is burning sensation, breach of skin is likely. Many national guidelines, for example, USA,[7] Canada, and Switzerland do not make a difference between category II and III wounds and recommend rabies vaccination alongwith RIG administration on potential exposure to rabid animals irrespective of the type of wounds. More such rabies death reviews may throw light on this unusual phenomenon of deaths due to scratches/abrasions by rabid animals, especially on the head, neck, shoulder region, hands and arms, in rabies endemic countries like India.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.