Can hives go away on their own

How long can hives last?
Hives can appear and disappear quickly, with each hive only lasting around 23 hours. However, depending on the cause, they may reappear and continue affecting someone for days, weeks, or longer.
People can have acute hives, which occurs due to a specific trigger and resolves within
This article looks at how long hives last, factors that influence their duration, and treatment.
Each hive lasts only
Acute hives appear quickly and do not last long. Doctors classify hives as acute if the overall duration is less than 6 weeks.
However, around 25% of people go on to develop chronic hives. This is when hives regularly reappear over 6 weeks or more.
For many individuals, chronic hives eventually clear on their own, but this can take months. According to the American Academy of Dermatology Association (AAD), around half of people with chronic hives spontaneously recover within 1 year.
Acute hives often occur in response to an allergen or irritant. When the immune system perceives a substance as a threat, it releases histamine and other chemicals. This causes tiny blood vessels under someones skin to leak fluid, which accumulates and causes the bump.
Some
- food allergens, such as milk, eggs, tree nuts, peanuts, or shellfish
- contact allergens, such as latex or animal dander
- insect bites or stings
- medications
Any drug can cause hives, but some of the medications most commonly associated with this symptom include:
Acute hives can also occur in response to viral infections, parasitic infections, or during times of stress.
According to a 2018 review, doctors are unsure of the cause of acute hives in
Chronic hives may have the same cause as acute hives, but with symptoms lasting longer than 6 weeks. However, chronic hives are often not due to an allergen and instead have a physical cause.
There are two subcategories of chronic hives: inducible urticaria and chronic idiopathic urticaria.
Chronic idiopathic hives
Chronic idiopathic urticaria has no clear cause and is the most common form of chronic hives. Researchers are working to understand why this type of hives occurs, but a leading theory links it with autoimmunity.
Autoimmunity occurs when a persons immune system mistakenly attacks healthy tissue, and several autoimmune conditions are associated with chronic hives. The most common is thyroid disease, which is present in
This suggests that the hives may result from someones immune system not functioning as it should. Other conditions that can occur alongside chronic hives include type 1 diabetes, lupus, and rheumatoid arthritis.
Infections can also be associated with the onset of chronic hives. This includes bacterial, viral, and parasitic infections. Again, this may result from autoimmunity an infection may trigger a change in how the persons immune system works.
Inducible hives
Inducible or physical urticaria is less common than chronic idiopathic urticaria. With this subtype, it is possible to purposely induce the hives by a person exposing their skin to certain triggers, which could include:
- Scratching or pressure: The
most common type of inducible hives is known as dermatographia. This condition involves developing hives as a response to scratching or drawing on the skin. - Cold: Cold hives occur on someones skin or mouth after exposure to cold temperatures. Triggers include consuming iced drinks, touching cold water, or going outside in cold weather.
- Heat: Cholinergic hives occurs when an individuals body becomes hot or sweaty. Hot baths, exercise, and spicy food can be triggers.
- UV light: Solar hives occur in response to UV light from the sun and certain light bulbs, such as those in tanning beds.
- Water: Some people develop hives if their skin comes into contact with water. This is known as aquagenic urticaria and is very rare.
Doctors diagnose hives by performing a physical examination. There is no test to determine whether the persons hives are acute or chronic, so they will use the length of time they recur to do this.
The doctor may also ask an individual:
- when the rash began
- the shape, size, and distribution of the rash
- where on the body they first noticed the rash
- if they have had any insect bites
- if they live or work with common hive triggers, such as chemicals, animals, or latex gloves
- if they have bone or joint pain, fever, or abdominal pain
- if anyone in their family experiences hives
- if they take any medications or supplements
The doctor may use a skin prick test and serum-specific IgE test to check if the acute hives result from a specific substance, such as food, dust mites, or chemicals. Alternatively, they may refer someone to an allergy clinic for these tests.
However, in cases of chronic hives, allergy testing is rarely useful. A doctor may check for other underlying health conditions by performing additional tests, such as:
The most suitable treatment depends on whether the person has acute hives or chronic hives.
Acute hives
Doctors typically recommend second-generation antihistamines as the first-line treatment for acute hives, such as:
- loratadine (Claritin)
- desloratadine (Clarinex)
- fexofenadine (Allegra)
- cetirizine (Zyrtec)
- levocetirizine (Xyzal)
They may prescribe a standard dose or increase by up to 4 times if the individual does not respond.
If these medications do not improve symptoms, the doctor may recommend an additional antihistamine, such as cimetidine (Tagamet), famotidine (Pepcid), or ranitidine (Zantac). They may recommend a 310-day course of corticosteroids to help control the symptoms in severe cases.
The doctor may prescribe an epinephrine auto-injector if they think the individual is at risk of anaphylaxis, which is a severe allergic reaction that restricts breathing. This provides emergency medicine to treat anaphylaxis quickly.
The doctor will then reassess the individual in 26 weeks.
Chronic hives
Doctors may recommend a four-step treatment plan for chronic hives. This approach involves using an antihistamine daily, which may be up to 4 times the regular dosage depending on how the individual responds.If necessary, they may prescribe a second antihistamine or another medication, such as montelukast (Singulair). With persistent hives, they may suggest a high potency antihistamine, such as hydroxyzine or doxepin.
The final step is for a doctor to refer the individual to a specialist for immunomodulatory therapy. This may involve taking medications such as omalizumab (Xolair) or cyclosporine (Sandimmune).
Once symptoms are under control, a doctor may gradually reduce the dosage of these medications. If the hives have an identifiable cause, such as cold or heat exposure, adopting changes to avoid the triggers wherever possible is also important.
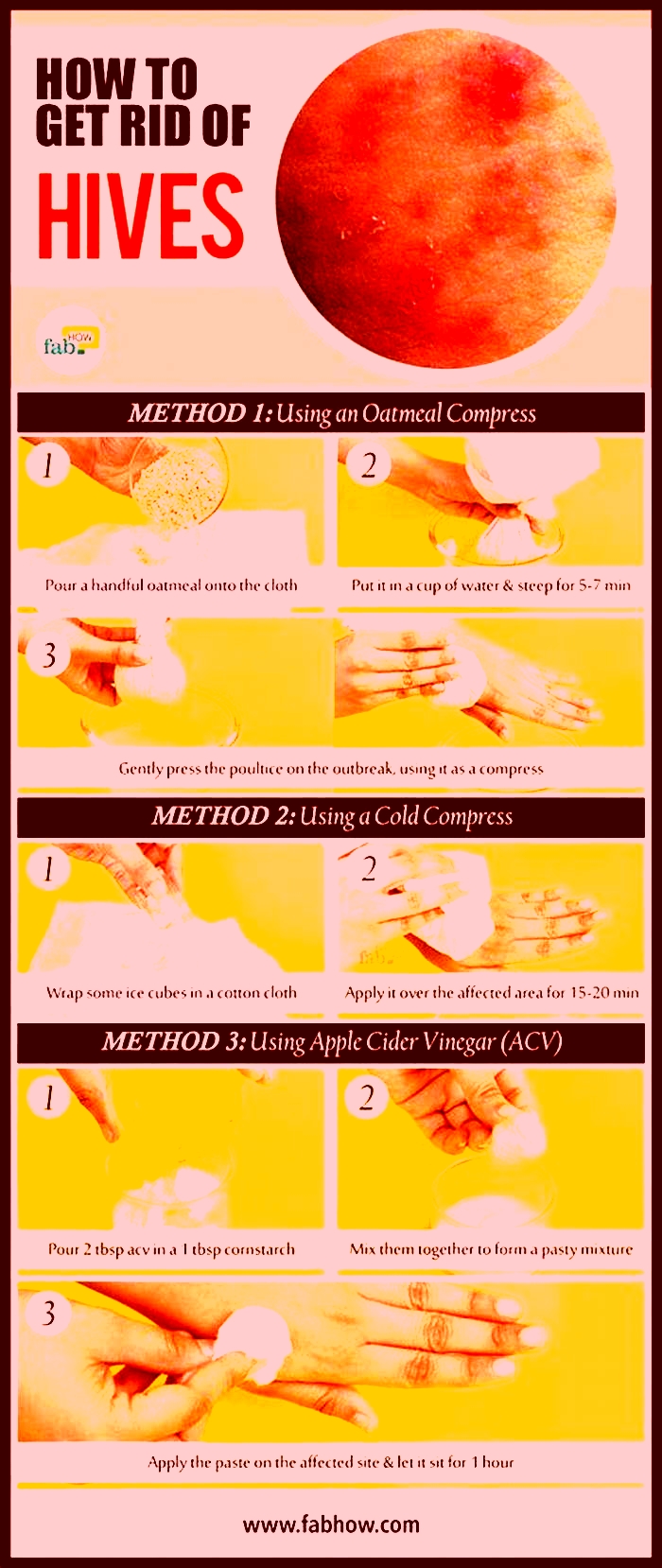
The AAD suggests the following methods for people to reduce irritation and itchiness in hives:
- applying topical anti-itch medications, such as calamine lotion
- wearing loose-fitting clothing
- moisturizing with fragrance-free lotion to prevent dry skin
- using cold compresses several times per day
However, it is important for individuals to try to determine whether the hives have a specific trigger, in addition to relieving symptoms. If someone has cold hives, for example, a cold compress may make them worse.
Therefore, it is a good idea for people to keep a symptom diary, recording when the hives occur and any factors that might have contributed. Symptom diaries are also useful to refer to at medical appointments. A person can take note of:
- the date and time the hives appear
- what they were doing just before they developed
- what they have had to eat or drink
If any common factors emerge when the hives occur, a person can try to temporarily avoid these to see if it helps. It is important for people to do this with the guidance of a doctor, allergist, or dietitian if someone has food-related hives.
Learn more about remedies and treatments for hives here.
Hives do not last long, taking only 23 hours to fade. However, more can appear, which makes the symptoms last longer. Acute hives can develop and resolve on their own within 6 weeks, while chronic hives can last much longer.
Doctors treat acute and chronic hives differently, so it is advisable for people to speak with a medical professional about this symptom, especially if the hives last longer than 6 weeks.
If hives or swelling occur in the mouth and airways, making it difficult to breathe, dial 911 or the number of the nearest emergency department immediately.
What Causes Hives That Recur Daily?
Hives that come back daily for 6 weeks or more are called chronic hives, or chronic urticaria. The condition often has no known cause, but allergies, autoimmune conditions, physical stimuli, and infections can play a role.
Hives are itchy, raised welts on the skin. They are often caused by an allergic reaction but might also have an unknown cause.
Hives that recur (go away and come back) frequently are known as chronic hives. Chronic hives of unknown cause can last for months or years. They can affect 1.4% of people, twice as often in women as in men.
Chronic hives can affect your quality of life, as severe itchiness can lead to discomfort and trouble sleeping. Yet treatment can help you manage them.
Lets look at the symptoms, possible causes, and treatment for hives that recur daily.
If you get new hives as others are clearing up for 6 weeks or more, you have chronic hives.
You can identify hives by their:
- raised patches or bumps on the skin
- itchiness on the patches or bumps
- stinging or burning sensation
- swollen skin appearance
Hives come in all different shapes and sizes, from just a small speck to several inches in diameter. A group of hives that appear in the same area is known as a plaque.
Medical emergencyCall emergency medical services or go to the nearest emergency room if you or someone youre with experience:
- sudden swelling of the lips, mouth, throat, or tongue
- fast breathing, choking, or wheezing
- trouble swallowing
- blue, gray, or pale color in lighter skin or on palms or soles of the feet in darker skin
- confusion, drowsiness, or dizziness
- inability to be woken up
Chronic hives look the same as other hives. Hives on light skin can appear pink or red. On dark skin, the color of the hives might be similar to the rest of your skin or slightly darker. Hives can also blanche on lighter skin, which is when a red hive becomes white if you press on it.
On all skin colors, hives are bumps or raised patches.
Chronic hives have many possible causes. Differences in symptoms, such as how quickly the hives appear, can help identify the cause.
Chronic idiopathic urticaria
Chronic idiopathic urticaria is when you get daily hives but doctors cant determine why. Symptoms include:
- hives that recur daily or nearly every day
- hives that last for 6 weeks or longer
- when each hive lasts 24 hours or fewer
- hives that do not bruise or scar your skin
Allergies
Hives can be triggered by exposure to a specific allergen.
Depending on the type of allergy, hives might come on quickly or over a few hours. Some common food allergens and the timing of related hives include:
- peanuts, shellfish, eggs, and nuts (hives often appear within 1 hour)
- bananas and chestnuts if you have a latex allergy (hives often appear within 1224 hours)
- food additives like colors and preservatives (hives often appear within 1224 hours)
Other types of allergies that might cause recurring hives include:
- insect bites or stings
- pet dander
- pollen
- certain plants
Autoimmune conditions
Several autoimmune conditions can cause chronic hives. Although researchers dont know exactly why this happens, chronic inflammation might
Among the autoimmune conditions that might cause hives are:
Infection or medication
If you have an infection or are taking medication, these might also lead to hives that recur daily. Examples include:
- Bacterial or viral infections:
- Medications:
When a doctor is trying to find the cause of your recurring hives, they might try to rule out infection or medication as a cause. Chronic hives last longer than 6 weeks, but an acute infection like the common cold might last less time than that.
A doctor might then look for another cause of your hives.
Physical stimuli
Your environment or certain activities can cause you to break out in hives. If these stimuli are a regular part of your life, it might lead to chronic hives.
Examples of stimuli that lead people to have hives almost immediately or within a few minutes include:
- cold
- heat
- ultraviolet light (outdoor sun exposure or tanning beds)
- vibration
- adrenaline (exercise or stress)
- water
- certain animals like jellyfish
Skin pressure from clothes or accessories can lead to hives right away or up to 424 hours later.
If you dont know the reason for your chronic hives, consider seeing a doctor. The hives might have a treatable cause like an allergy or physical stimulus. Treatment can relieve symptoms even if the cause is unknown.
Also consider seeing a doctor if hives:
- do not get better after 2 days
- seem to be spreading
- accompany high temperature
- accompany a feeling of unwellness
- accompany swelling under the skin
A doctor, usually a specialist such as an allergist, diagnoses chronic hives by:
- taking a medical history
- asking about your symptoms
- performing a physical exam
- conducting an allergy patch test
If your chronic hives are from a specific trigger, avoiding that trigger might make them go away.
Self-care options include:
- applying cool compresses
- using anti-itch creams or ointments
- bathing in colloidal oatmeal
- wearing loose-fitting clothes
- avoiding scratching
- using fragrance-free, gentle skin cleansers
Medications include:
- antihistamines (prescription or over-the-counter)
- corticosteroids
- omalizumab (injectable medication)
- phototherapy
Chronic hives can go away without treatment. About half of people with chronic hives no longer experience them within a year.
Here are some answers to common questions about chronic hives.
Why do I keep getting hives every day?
Chronic hives can have a variety of causes, including allergies, autoimmune conditions, infections, or physical stimuli. Many cases of chronic hives have no known cause.
What do autoimmune hives look like?
Autoimmune hives appear as raised, itchy patches of skin or bumps. They might appear pink or red on light skin and on dark skin as a bit darker than the rest of your skin. Hives can be of any size or shape.
When should I be worried about recurring hives?
You should consider seeing a doctor whenever you have hives that keep coming back. A doctor might be able to help you find a cause. Even if the cause is unknown, treatments such as antihistamines and self-care can help improve your symptoms.
Treatment for chronic hives with antihistamines, corticosteroids, light therapy, and home care can help improve symptoms.