Do hives get worse before they get better

When is a drug rash more than just a rash?

You were recently started on antibiotics for an infection and you are now doing well. But slowly your skin begins to itch, and the telltale signs of a rash are already popping up first on your torso, and now spreading to your arms and legs. What do you do? Should you worry? Should you see a medical professional?
Rashes are a common and pesky side effect of many medications. It can be so disheartening to be getting better from one ailment only to discover that you have another issue to address. While these itchy eruptions can be annoying, they usually run their course over a week or two and can be treated with topical medications.
But not all drug rashes are created equal and some can even be deadly. Luckily the scary ones are pretty rare, but it's still a good idea to know how to spot them. How can you tell the serious rashes from ones that are just a nuisance, but will get better with time and treatment?
Types of drug rashes
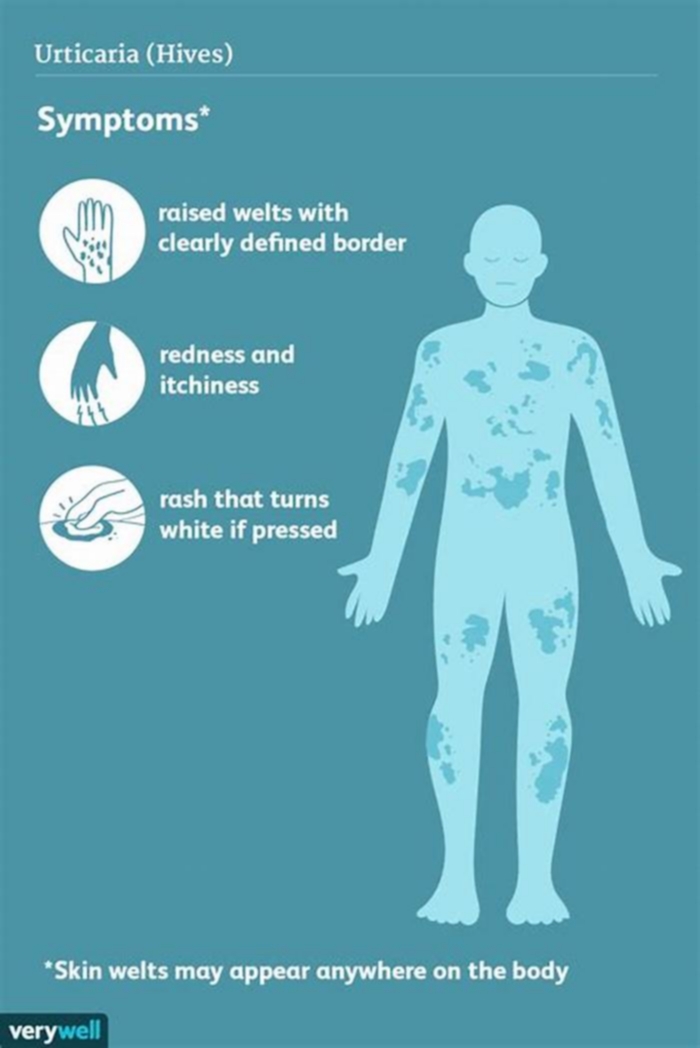
There are two main allergic rashes that may happen after taking a drug. The most immediate type of reaction happens within hours. Hives appear and move around the skin. Since this process is related to the release of histamine, antihistamines (available over the counter at a drugstore) are the typical treatment.
There is also a delayed type of drug rash that comes up four to 14 days after you start taking a medication. Pink and red bumps appear on your chest and back, and spread to the arms and legs over the course of days. Unlike hives, these bumps don't move around, and after a few days things may start to get better, but you may have peeling skin much like a healing sunburn.
This delayed type of rash doesn't respond as well to antihistamines, but an over-the-counter topical cortisone cream (or one of its stronger prescription-strength versions) can help speed the healing process along.
When is a drug rash cause for concern and a visit to the ER?
With hives, the main concern is that you're experiencing a whole-body reaction that goes beyond the skin, one that can make breathing difficult or dangerously drops your blood pressure. If you experience either of these symptoms, it's very important to get to the ED.
These immediate, life-threatening reactions can be treated with steroids, epinephrine, and higher-dose antihistamines than you can find at the drug store. While they are scary, these types of allergic reactions to a drug are not hard to identify, and many doctors are skilled at spotting dramatic changes in your breathing or blood pressure. It's important to tell the doctor you see what medications you have taken and how long ago you took them.
Know the signs of severe cutaneous adverse reactions (SCARs)
In the more delayed type of rash, symptoms can be more difficult to diagnose. The most common triggers for these types of rashes include antibiotics, antiseizure medications, antigout medications like allopurinol, and even over-the-counter medications like NSAIDs. (This isn't a complete list, and any new medication should be regarded with caution.)
As for the rash, when it's just itching things are usually fine, but still a nuisance. When the skin starts to hurt, or turns a deeper purple color, doctors worry about something more serious. If your skin starts to blister up or you see pustules, or if you notice sores in your mouth, eyes, or your genitalia, these are red flags and you should get to an urgent care clinic or the ER and ask for a dermatology consultation. Sores in the mouth can be so severe that drooling becomes a common symptom, because patients avoid swallowing due to the pain.
If you start to feel ill, like you have the flu, or if you're getting puffy from swelling, especially in the face, this could mean it's a severe drug hypersensitivity syndrome. Sometimes people develop a fever, a drop in their blood pressure, or their liver, kidneys, and heart can all be affected by drug hypersensitivity syndromes. These are so severe that most patients need to be admitted to the hospital, and sometimes even to the burn or intensive care unit.
While there are different names for different types of severe drug reactions, including Stevens-Johnson syndrome (SJS), drug rash with eosinophilia and systemic symptoms (DRESS), and acute generalized exanthematous pustulosis (AGEP), they are often grouped together as severe cutaneous adverse reactions (SCARs).
What happens if you develop a SCAR from a medication?
The first step is getting evaluated by a specialist, either in a dermatological clinic or the hospital. Finding someone who has expertise in managing these types of reactions is critical. A doctor (usually a dermatologist) may biopsy your skin, and they may have to start systemic medications that suppress your immune system. Sometimes, patients with SCARs also require a stay in a hospital.
The most important thing you can do is to keep an eye on your skin and its symptoms if you're taking a new medication, or even if you've increased the dose of an old medication. If you suspect that you may be dealing with one of these SCARs, be sure to seek help from an expert, like a board-certified dermatologist, so that you can rest assured that you're getting the care you need. Patients who are treated appropriately generally do well. Your doctors should also report these reactions to the FDA.
Once you're on the mend, things can start to get back to normal, but it's important to follow up with your doctors because there are some long-term issues that are important to pay attention to. Ultimately your doctors and healthcare team will advise you on what exactly is safe in the future. Remember that if you're worried about one of these reactions, it's important to stop the medication as soon as possible, but with the input of your doctors.
Why It's Better to Face Your Problems
One of the greatest struggles in therapy is reconciling the motivation to avoid with the need to approach something difficult. It is understandable that when someone is afraid of something, they want to avoid it. When someone feels depressed about something, they may find it easier to not think about why they are depressed than to face the problem and try to solve it. But, long term, such avoidance leads to more depression and more anxiety.
Lets start with some definitions (sorry). "Avoidance" is when someone does not engage with a problem, situation, or person. Avoidance can be behavioral, where the person physically disengages, or it can be cognitive, which involves attempts to not think about the problem or situation. Avoidance is often contrasted with "approach." Approach means facing the problem or situation, trying to generate and use solutions, and can also be thought of as coping or dealing with the problem. Just because someone is approaching a problem does not guarantee that their strategies are effective, but, in general, approaching a problem versus avoiding it is more helpful.
Avoidance can play a role in perpetuating anxiety and depression. With anxiety, there is a strong tendency to avoid things we fear. However, avoiding these things too often means we dont learn how to face these problems or situations and dont learn our own strengths. This means we accrue less evidence that we can face these problems and more anxiety the next time the problem comes up. Something similar happens with depression. A person with depression may avoid social gatherings or other activities but this can lead to more depressed feelings because those same activities could counteract depression. For both depression and anxiety, avoidance is a key factor in preventing symptoms from getting better.
Approaching a problem leads to a temporary increase in anxiety but avoidance can lead to long term anxiety
Source: Salene Jones
Given the harmful effects of avoidance, it might seem odd that people continue to avoid. One reason we do this is that it often gets worse before it gets better. Approaching problems is tough and can lead to a temporary increase in anxiety or sadness. Over time, as a person copes with a problem and learns they do have the strength and skills, the anxiety and sadness fade. But that temporary increase can be difficult to overcome, even when avoidance leads to more anxiety and sadness long term. (The different trajectories are shown in the graph.)
This relationship between avoidance and approach is similar to the relationship between difficult truths and lies. Facing a difficult truth may hurt more now, but lies hurt forever. Learning how to cope with and get past that initial hurt is key to feeling better.
As with anything psychological, there are caveats. Just because someone is not facing a problem, situation, or person does not necessarily mean they are avoiding it. In abusive relationships, the way to face the problem may be to limit or stop contact with the abusive person. It might look like someone is avoiding a problem when limiting contact with an abusive person, but it is actually approaching the problem and setting boundaries.
Sometimes people do not have the capacity to approach a problem. They might have more bandwidth in the future, but if they are too stressed, tired, or emotionally drained, it would not make sense to approach the problem. Trying to face a problem when one does not have the capacity could set someone up for failure. Temporary avoidance, used judiciously, can actually help a person face their anxiety and depression later and slowly start to feel better.
The overall strategy should be to approach problems in whatever way makes the most sense for the situation.
Facebook image: Hector Pertuz/Shutterstock
LinkedIn image: Yandry_kw/Shutterstock
Hives Symptoms: What They Look Like
Hives are characterized by red or pale-colored welts on the skin, which typically come and go throughout the day, says Sourab Choudhury, DO, a dermatologist and the chief medical officer at the Dermatology Specialists, a private dermatology practice in New York City. Sometimes they itch, burn, or sting.
Usually the welts will be surrounded by clear edges. They may look similar to bug bites, but hives generally will appear and disappear more quickly. They may itch, sometimes severely, and theyre not always the same size or shape. They may be as small as the tip of a pen or as large as a dinner plate. (4) When you press the center of a hive bump on the skin, it likely will turn from red to white, which is known as blanching. (2,3)
Hives may appear on the body grouped together and take over a large area of the skin, or as a couple of individual welts that show up here and there. (4) They can appear anywhere on the body, though some people get them in the same spot over and over again (usually as a result of a specific trigger). (4)
Generally, youll know you have hives simply by seeing the hives themselves. If you experience other symptoms, such as swelling in the eyes, lips, or inside of the throat, or if you have trouble breathing, you should call 911 or see a doctor immediately, says Sapna Palep, MD, a dermatologist at Spring Street Dermatology in New York City. These symptoms indicate you may be experiencing a serious allergic reaction called anaphylaxis. (5)
Why It Gets Worse Before It Gets Better

When I first heard that once I started really digging into my trauma, things would get worse before they got better, I thought I understood. I thought it meant that acknowledging my pain would cause me more pain at first, but then it would heal and I would be "better." I knew that was a naive way of looking at things, but I still believed that would generally be the process. Boy, was I wrong.
How It Gets Worse Before It Gets Better
I thought things would get worse before they got better at first because acknowledging pain is hard, but it turns out there's so much more to it than that. Right now, my mental health is doing a lot worse than it was a few months ago because I've been really digging into my trauma recovery. Yes, acknowledging my trauma has been hard, but what's really been making my mental health worse is the onslaught of intrusive thoughts I've been dealing with the last few weeks. Without wanting to or meaning to, I think about hurting myself and my baby almost every day.
I thought I was losing it, so I brought it up with my therapist, and she said this is what people mean when they say it gets worse before it gets better. She said these intrusive thoughts are my brain's way of fighting to keep the status quo. All change is threatening to our brains, especially to traumatized brains, so they fight our efforts to improve with whatever tools they have. In my case, it's lots of scary thoughts.
Have you noticed your mental illness getting worse when you've tried really hard to heal or recover? How have you dealt with the surge of symptoms? Share your story about how it's gotten worse before getting betterin the comments,and check out more of my story in the video below.
APA ReferenceGriffith, M. (2020, August 11). Why It Gets Worse Before It Gets Better, HealthyPlace. Retrieved on 2024, April 26 from https://www.healthyplace.com/blogs/recoveringfrommentalillness/2020/8/why-it-gets-worse-before-it-gets-better