Do you need antibiotics after a dog scratch

Do you need a tetanus shot for a dog scratch? A Step-by-Step Guide
What to Do:
- the wound is on the face, neck, hand, foot, or near a joint
- the wound wont stop bleeding after 10 minutes of direct pressure
- the wound appears to be deep, large, or severe
- the attacking animal was stray or wild or behaving strangely
- the bite or scratch has pus coming from it, or becomes red, hot, swollen, or increasingly painful
- your child has a weakened immune system or other medical condition that might make an infection more likely
- your childs tetanus immunizations are not up to date
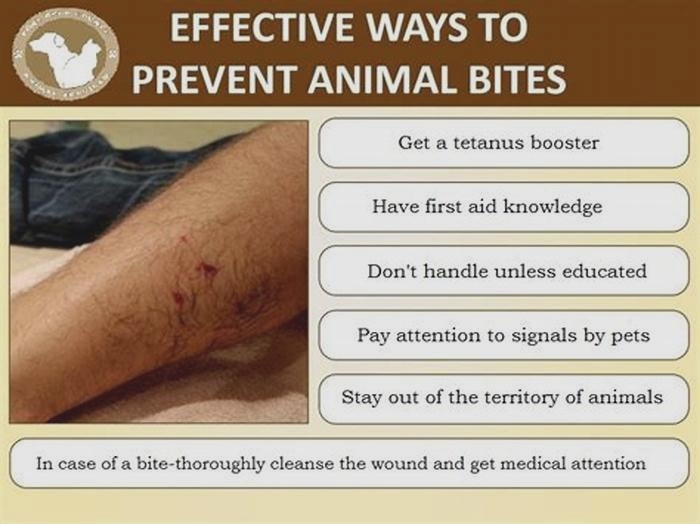
Teach your children to stay away from strange animals, and not to tease or provoke any animals, even family pets. Animals should not be disturbed while they are eating or sleeping.
If you own a pet, make sure its properly immunized and licensed.
Signs of an infection from a scratch wound
While your dog scratch wound heals, look for the following possible signs of an infection:
See a doctor if you notice any signs of infection from a dog scratch.
Some dogs carry a bacteria in their mouths called Capnocytophaga. While these bacteria rarely spread to people, theres still a chance of getting sick from exposure to an animals saliva, especially if you have a weakened immune system.
Capnocytophaga infections can progress quickly, even becoming life-threatening. Possible symptoms related to this type of infection include:
Call or visit a doctor if youre experiencing any signs of infection post-dog scratch. Its also a good idea to seek medical attention any time youve been scratched by a dog especially if the dog isnt your own.
In the case of a dog bite, you should seek medical care to rule out the risk of rabies and other potentially life-threatening diseases.
Rabies is a type of viral infection that can occur when bitten by an animal thats infected. This is a serious infection that can be fatal in both animals and humans, due to the viruss attack on the nervous system.
While animal-to-animal transmission is possible, its not as common for humans to be infected by household pets in the United States. Part of this reduced risk is attributed to rabies vaccines in domesticated animals.
Still, rabies ought to be considered in the case of a serious wound from a dog, particularly if its a stray dog or one who hasnt been vaccinated against rabies. The virus may be transmitted through an infected dogs saliva from biting or accidental scratching.
Can you get tetanus from dog scratch?
Potential Infections Can Occur from a Dog Scratch
Dogs walk on all four feet and dig in whatever they can find, which means dog nail beds are very dirty. They can harbor all sorts of bacteria and fungi that can readily infect humans through broken skin, including tetanus.
When to get a Tetanus Shot | Can you get Tetanus from a Scratch
Animal bites and scratches are extremely common, although often overlooked in terms of potential severity. Even a minor bite or scratch from an animal of any kind can become infected with bacteria that may be harmful, occasionally leading to serious complications. While scratches and bites may not look angry or infected, this is not to say that they dont come along with plenty of risksincluding the risk of tetanus.
As one might expect, animal bites and scratches can occur at any time and are highly dependent upon circumstance. Dog bites, for example, are common and account for 98% of rabies cases reported worldwide. Cat scratches and bites are equally common, and despite what many may think, theyre actually more likely to result in infection than dog bites.
Finally, scratches and bites from wild animals such as raccoons, coyotes, skunks, foxes and batsall of which are cause for concernoccur regularly and should always be addressed by a medical professional no matter how mild or severe they may be.
Symptoms of animal bites and scratches can vary quite dramatically depending upon the severity of the incident. These may include the following:
The first step in diagnosing an animal bite or scratch is for you and your treating provider to have a discussion about exactly how the injury happened. From there, an approach to treatment will be discussed. The wound will most commonly be cleaned and dressed to avoid any potential for infection (wounds missing skin or those that are particularly deep may require special dressings). Stitches may also be employed if necessary. Antibiotics may be prescribed to reduce the risk of infection.
In the case that the affected person is not up to date on their tetanus shot, a vaccine may be administered as a prophylactic.
Children who experience symptoms after suffering an animal bite or scratch should be seen by a treating provider as soon as possible after the injury. For children that have not been vaccinated, a tetanus shot may be provided.
At ConvenientMD, we encounter animal bites and scratches numerous times each and every day. While many can be treated quickly and efficiently, complications do arise and can only be avoided when injuries are addressed as soon as possible. If you or a family member has been bitten or scratched, were here to help.
Ready to get treated? Just stop into any of our convenient urgent care locations in New Hampshire, Maine, and Massachusettsyoull never need to make an appointment ahead of time.
Treatment for Dog and Cat Bites and Scratches
Treatment for Dog and Cat Bites and Scratches
How to deal with dog or cat bites and scratches
When your child is bitten or scratched by an animal, be calm and reassure your child that you can help. Your child's healthcare provider will determine specific treatment for an animal bite. Treatment may include:
For shallow bites from a household pet that is immunized and in good health:
Wash the wound with soap and water under pressure from a faucet for at least5 minutes. Dont scrub as this may bruise the tissue. Apply an antiseptic lotion or cream.
Watch for signs of infection. These include fever, increased redness or pain, and swelling, or fluid leaking, or red streaks from the bite. Call your child'shealthcare provider right away if any of these occur.
For deeper bites or puncture wounds from any animal, or for any bite from an unknown animal:
If the bite or scratch is bleeding, apply pressure to it with a clean bandage, cloth, or towel to stop the bleeding. If bleeding doesn't stop after 15 minutes of pressure, call your healthcare provider.
Wash the wound with soap and water under pressure from a faucet for at least5 minutes. Dont scrub as this may bruise the tissue.
Dry the wound and cover it with a sterile dressing. Dont use tape or butterfly bandages to close the wound. This could trap harmful bacteria in the wound.
Call your child's healthcare provider for help in reporting the attack and to decide if more treatment is needed. This may include antibiotics, a tetanus booster, rabies vaccine, or repair of the wound with stitches. This is very important for bites on the face or for bites that cause deeper skin puncture wounds. It is important to tell your child's healthcare provider about all cat bites, especially around the hands and wrist. These injuries are known for often causing infection.
If possible, find the animal that caused the wound. Some animals need to be captured, confined, and closely watched for rabies. Dont try to capture the animal yourself. Instead, contact the nearest animal warden or animal control office in your area.
If the animal can't be found oris a high-risk species (raccoon, skunk, or bat), or the animal attack was unprovoked, your child may need a series of rabies shots.
Call your child'shealthcare provider for any flu-like symptoms after an animal bite. These symptoms may include fever, headache, ill feeling, loss of appetite, or swollen glands.
What to Do If a Dog Scratches You
Many people know about cat scratch fever, but can a dog scratch be just as dangerous? Although you are less likely to contract severe illness from a dog scratch, there is still a possibility of it happening. If you are scratched by a dog, heres what you need to know.
Potential Infections Can Occur from a Dog Scratch
Dogs walk on all four feet and dig in whatever they can find, which means dog nail beds are very dirty. They can harbor all sorts of bacteria and fungi that can readily infect humans through broken skin, including tetanus. Dogs also lick their paws, transferring bacteria from the mouth onto the nails. This can, in rare cases, infect humans with MRSA or bacteria called Capnocytophaga if the scratch breaks the skin.
What About Rabies?
Can I get rabies from a dog scratch? is a popular online search. Even though it is highly unlikely that a human will contract rabies from an animal scratch, it can still happen. The virus that causes rabies is spread through contact with saliva or brain tissue from an animal infected with rabies, but it cannot penetrate unbroken skin. If a rabid dog with saliva-covered nails scratches a human, theoretically infection can occur; however, most dogs are vaccinated against rabies and are not at risk for infection. If your dog has had contact with a rabid animal, take additional precautions and seek veterinary care immediately.
How to Treat a Dog Scratch
Animal scratches may seem harmless, but they can turn into serious infections if the skin is broken. Puncture wounds may look the least serious, but they carry the highest risk of severe infection. If the scratch is bleeding heavily, apply pressure with a clean towel until the bleeding has stopped. Once the bleeding has subsided, wash the wound thoroughly with soap and water for three minutes. Clean and dry the skin, and then apply a small amount of antibiotic ointment and cover the wound with a bandage. Make sure to check the scratch for signs of infection, which include increased heat, redness, swelling, pain or red streaking on the skin. Monitor the wound for at least 72 hours, and if you experience any of those symptoms, seek the attention of a medical professional immediately.
WRITTEN BY
Sarah Wooten, DVMVeterinarian
Dr. Sarah Wooten graduated from UC Davis School of Veterinary Medicine in 2002. A member of the American Society of Veterinary Journalists,...
ANIMAL BITES OVERVIEW
Animal bites are a common problem in the United States, with two to five million occurring each year. The vast majority of animal bites are caused by dogs (85 to 90 percent), with the remainder caused by cats (5 to 10 percent) and rodents (2 to 3 percent). Children are bitten more often than adults.
The most feared complication of an animal bite is rabies, although skin infection is the most common complication. Some bite wounds can be serious, causing injury and permanent disability. Bite wounds to the hand carry an especially high risk for serious complications because the skin's surface is so close to the underlying bones and joints.
This topic review discusses recommendations for care after an animal bite. Prevention of rabies is discussed in a separate topic review. (See "Patient education: Rabies (Beyond the Basics)".)
TYPES OF ANIMAL BITES
The location and type of the injury depends upon the animal inflicting the bite.
Dog bitesVictims of dog bites frequently know the dog that attacked them. Most dog bites occur in children, with the highest number seen in boys between the ages of five and nine years old. The head and neck are the most common site of bites in children up to age 10 years, probably because a child's head is close to the level of a large dog's mouth. The arms and legs, particularly the right hand, are the most frequent site of injury for older children and adults. A dog bite can lead to a range of injuries, including scratches, deep open cuts, puncture wounds, crush injuries, and tearing away of a body part. Dog bites rarely cause death.
Certain breeds of dog are more commonly associated with bites. German Shepherds, pit bull terriers, and mixed breeds account for the majority of dog bite injuries.
Cat bitesCats can cause wounds with their teeth or claws. Two-thirds of cat bites involve the upper extremities (arms and hands). Scratches typically occur on the upper extremities or face.
Deep puncture wounds are of particular concern because cats have long, slender, sharp teeth. When the hand is bitten, bacteria can get into the tissue that surrounds the bones or into a joint and result in osteomyelitis (infection of the bone) or septic arthritis (infection of the joint).
If infection occurs, it generally progresses rapidly, causing skin redness, swelling, and intense pain as quickly as 12 to 24 hours after the bite.
Rodent bitesRats cause the majority of rodent bites. Most bites occur at night on the face or hands in children five years old or younger.
Human bitesChildren are the most common victims of human bites, usually as a result of aggressive play with another child. Human bites can cause a semicircular or oval area of skin redness or bruising, and the skin may be punctured. Human bites are typically located on the face, upper extremities, or trunk (chest or abdomen).
Other types of bitesThe bites of most other animals, such as squirrels, rabbits, and guinea pigs, are generally treated the same way as cat bites.
ASSESSING FOR RABIES EXPOSURE
Contacting your local public health agency immediately can be valuable to help you understand the risk of transmission after a potential exposure and determine whether postexposure prophylaxis is needed.
Because cats and dogs may harbor rabies, all cat and dog bites should be reported to the animal control section of the local health department as soon as possible. The cat or dog should be quarantined for 10 days and tested for rabies if concerning behavior develops. If quarantine is not possible, or if you are bitten or scratched in a country where rabies is common, you should seek expert advice about the need for postexposure prophylaxis. (See "Patient education: Rabies (Beyond the Basics)".)
Anyone who is bitten or scratched by a raccoon, skunk, fox, coyote, or bat needs immediate medical attention, even if the bite is small and does not appear to be infected. These animals can be carriers of rabies, and since it's typically not possible to know for certain whether a wild animal is carrying rabies, the person who was bitten or scratched should receive postexposure rabies immunization as soon as possible.
When a bite or scratch occurs in a foreign country, you should seek immediate attention in that country and upon your return home.
ANIMAL BITE TREATMENT
After being bitten by an animal or human, it is important to quickly and thoroughly clean the wound with soap and a large amount of water; this can help to prevent infection. If there is bleeding, a clean towel or gauze should be pressed to the wound to slow or stop the bleeding.
Do I need treatment?Adults or children who have been bitten by an animal or human should see a health care provider if:
An animal bite has broken through the skin and bleeding does not stop after applying pressure for 15 minutes
A bone may be broken, or if there is other serious injury
Cosmetic damage is a concern
A bite victim has diabetes, liver disease, cancer, HIV-infection, or takes a medication that could weaken the immune system
It is best to be evaluated and treated as soon as possible after being bitten to reduce the chance of developing an infection. This is particularly true if the bite occurs in resource-limited countries where animal vaccination programs to prevent rabies are not prevalent.
People who do not meet the above criteria should watch their wound carefully for signs of infection (eg, worsening pain, redness or warmth, fever, or pus-like discharge); if the bite is near a joint, the person should monitor for pain, swelling, and joint movement. Anyone whose wound appears to be worsening rather than improving should seek medical care. It is not necessary to be evaluated after a cat scratch from a house pet unless there are signs or symptoms of infection (worsening pain, warmth or redness, pus-like discharge, or fever). If the scratch originates from an unknown cat from the outdoors that attacked without provocation, medical advice should be sought regarding rabies risk. (See "Patient education: Rabies (Beyond the Basics)".)
AntibioticsThe most common complication of an animal bite is infection. Antibiotics are generally recommended to prevent infection in people with high-risk wounds, such as deep puncture wounds, wounds involving a bone or joint, and for people with other health problems, such as a weakened immune system or diabetes, which could increase the risk of serious infection.
Many experts also recommend antibiotics for any person bitten by a cat because there is a high rate of infection from cat bites.
Antibiotics are usually given by mouth as a pill or liquid. If the wound becomes infected, some people will require intravenous antibiotics or a more prolonged course of oral antibiotics.
Tetanus immunizationTetanus is a serious, potentially life-threatening infection that can be transmitted by an animal or human bite. Adults who are bitten should receive a tetanus vaccine (called a tetanus toxoid vaccine) if the most recent tetanus vaccine was greater than 5 years previously. (See "Patient education: Vaccines for adults (Beyond the Basics)".)
Children should receive a tetanus vaccine in the following circumstances:
They have received less than three doses of vaccine.
The wound is clean and it has been greater than 10 years since the last dose of tetanus vaccine for clean minor wounds.
The wound is dirty and it has been greater than five years since the last dose of tetanus vaccine.
In addition, if the wound is contaminated, tetanus immune globulin may be recommended if the person has had fewer than three tetanus vaccines or doesnt know. The tetanusimmune globulin provides additional protection against tetanus infection.
Rabies immunizationPeople who are bitten by an animal that could be infected with rabies MUST seek medical attention immediately to determine if a series of injections is needed to prevent rabies, which is, for the most part, a fatal illness. This is discussed in detail in a separate topic review. (See "Patient education: Rabies (Beyond the Basics)".)
Sutures (stitches)Some wounds can be sutured (stitched closed) within several hours of the injury, after the wound is thoroughly cleaned. Wounds to the face are usually closed immediately to avoid developing a scar.
However, due to the risk of infection, some bite wounds may not be sutured immediately. These wounds may be left open and sutured 72 hours after the injury. When wounds are left open, they are flushed with saline (a salt and water solution), left open to drain, covered with a dressing, and examined daily to look for signs of infection.
Immediate suturing may not be recommended for wounds at high risk of becoming infected, including:
Crush injuries
Puncture wounds
Bites involving the hands
Dog bite wounds that occurred many hours earlier
Cat or human bites, except those to the face
Bite wounds in people who have a weakened immune system
Management of an infected bite woundRegardless of initial management, some people will end up with an infection to their wound. If this happens, the wound may need to be opened and have pus drained, and antibiotics may be required. People with an infected wound can be treated at home unless the person is not able to take care of their wound or if there is concern that the infection is worsening; in these cases, hospitalization is recommended.
People who are at risk for developing a wound infection should seek prompt medical attention even if there are no signs of redness (see 'Do I need treatment?' above). For example, a person who has a deep puncture wound in their hand from a cat bite should seek medical attention immediately to prevent infection. Medical care usually consists of cleaning and dressing the wound and oral antibiotics that can be taken at home.
An X-ray may be done to ensure that there is no bone fracture and that tooth fragments are not buried in the wound. Infected bite wounds are not generally sutured immediately. Severe wound infections may require antibiotics given by intravenous injection and/or hospitalization.
SUMMARY
Adults or children who have been bitten or scratched by an animal or human should see a health care provider in the following situations:
An animal has bitten and broken the skin and bleeding does not stop after applying pressure for 15 minutes, a bone may be broken, or there is other serious injury.
A dog or cat has bitten the hand, foot, or head, or has bitten another area and caused a large wound.
A bite victim has diabetes, liver disease, cancer, HIV infection, or takes any medications that could weaken the immune system.
There are signs or symptoms of infection, including worsening pain, warmth or redness, pus-like discharge, or fever.
If the bite victim had their last tetanus shot more than five years ago, or if they cannot remember when they received their last tetanus shot. (See "Patient education: Vaccines for adults (Beyond the Basics)".)
If there is a concern about possible rabies. This is particularly true for travelers in certain resource-limited countries where animal vaccination programs to prevent rabies are not commonplace.
WHERE TO GET MORE INFORMATION
Your health care provider is the best source of information for questions and concerns related to your medical problem.
This article will be updated as needed on our website. Related topics for patients, as well as selected articles written for health care professionals, are also available. Some of the most relevant are listed below.
Patient level informationUpToDate offers two types of patient education materials.
The BasicsThe Basics patient education pieces answer the four or five key questions a patient might have about a given condition. These articles are best for patients who want a general overview and who prefer short, easy-to-read materials.
Patient education: Animal and human bites (The Basics) Patient education: Avoiding infections in pregnancy (The Basics) Patient education: Taking care of cuts, scrapes, and puncture wounds (The Basics) Patient education: Swollen neck nodes in children (The Basics) Patient education: Tetanus (The Basics) Patient education: Cat scratch disease (The Basics)
Beyond the BasicsBeyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are best for patients who want in-depth information and are comfortable with some medical jargon.
Patient education: Rabies (Beyond the Basics) Patient education: Vaccines for adults (Beyond the Basics)
Professional level informationProfessional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings. These articles are thorough, long, and complex, and they contain multiple references to the research on which they are based. Professional level articles are best for people who are comfortable with a lot of medical terminology and who want to read the same materials their doctors are reading.
Pasteurella infections Rabies immune globulin and vaccine Rat bite fever Animal bites (dogs, cats, and other mammals): Evaluation and management Human bites: Evaluation and management Indications for post-exposure rabies prophylaxis Zoonoses: Cats Zoonoses: Dogs Zoonoses: Animals other than dogs and catsThe following organizations also provide reliable health information.
National Library of Medicine
(https://www.nlm.nih.gov/medlineplus/animalbites.html, available in Spanish)
Centers for Disease Control and Prevention (CDC)
Toll-free: (800) 311-3435 (www.cdc.gov)
[1-12]