Does ibuprofen help with hives

Hives and angioedema
Overview
Hives
Hives
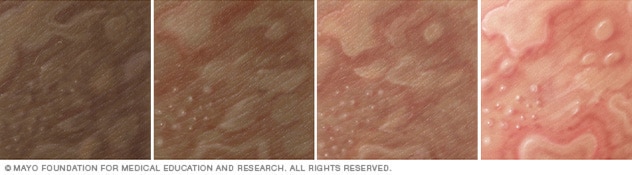
Illustration of hives on different skin colors. Hives can cause swollen, itchy welts. Hives is also called urticaria.
Angioedema
Angioedema
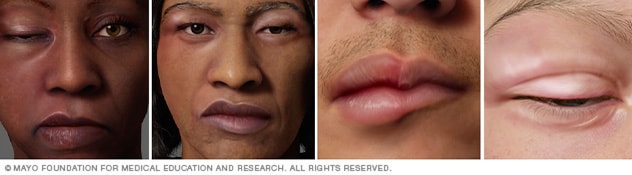
Illustration of angioedema on different skin colors. Angioedema causes swelling in the deeper layers of skin, often of the face and lips. It often goes away within a day.
Hives also known as urticaria (ur-tih-KAR-e-uh) is a skin reaction that causes itchy welts that range in size from small spots to large blotches. Hives can be triggered by many situations and substances, including certain foods and medications.
Angioedema can arise with hives or alone. It causes swelling in the deeper layers of skin, often around the face and lips. Short-lived (acute) hives and angioedema are common. Most times, they are harmless, clear up within in a day and don't leave any lasting marks, even without treatment. Hives that last longer than six weeks are called chronic hives.
Hives and angioedema are usually treated with antihistamine medication. Angioedema can be life-threatening if swelling of the tongue or in the throat blocks the airway.
Symptoms
Hives
The welts associated with hives can be:
- Skin-colored, reddish on white skin, or purplish on black and brown skin
- Itchy, ranging from mild to intense
- Round, oval or worm-shaped
- As small as a pea or as large as a dinner plate
Most hives appear quickly and go away within 24 hours. This is known as acute hives. Chronic hives can last for months or years.
Angioedema
Angioedema is a reaction similar to hives that affects deeper layers of the skin. It can appear with hives or alone. Signs and symptoms include:
- Welts that form in minutes to hours
- Swelling, especially around the eyes, cheeks or lips
- Mild pain and warmth in the affected areas
When to see a doctor
You can usually treat mild cases of hives or angioedema at home. See your health care provider if your symptoms continue for more than a few days.
If you think your hives or angioedema was caused by a known allergy to food or a medication, your symptoms may be an early sign of an anaphylactic reaction. Seek emergency care if you feel your tongue, lips, mouth or throat swelling or if you're having trouble breathing.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
ErrorEmail field is required
ErrorInclude a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Causes
For most people who experience acute hives and angioedema, the exact cause can't be identified. The conditions are sometimes caused by:
- Foods. Many foods can trigger reactions in people with sensitivities. Shellfish, fish, peanuts, tree nuts, soy, eggs and milk are frequent offenders.
- Medications. Many medications may cause hives or angioedema, including penicillins, aspirin, ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve) and blood pressure medications.
- Airborne allergens. Pollen and other allergens that you breathe in can trigger hives, sometimes accompanied by upper and lower respiratory tract symptoms.
- Insect bites and infections. Other causes of acute hives and angioedema are insect bites and infections.
Risk factors
Hives and angioedema are common. You may be at increased risk of hives and angioedema if you:
- Have had hives or angioedema before
- Have had other allergic reactions
- Have a family history of hives, angioedema or hereditary angioedema
Complications
Severe angioedema can be life-threatening if swelling of the tongue or in the throat blocks the airway.
Prevention
To lower your likelihood of experiencing hives or angioedema, take the following precautions:
- Avoid known triggers. If you know what has triggered your hives, try to avoid that substance.
- Bathe and change your clothes. If pollen or animal contact has triggered your hives in the past, take a bath or shower and change your clothes if you're exposed to pollen or animals.
Oct. 27, 2023
10 ways to get relief from chronic hives
 Biosimilars: 14 FAQs
Biosimilars: 14 FAQsFind answers to questions patients ask about this newer treatment option, including, Whats involved in switching from a biologic to a biosimilar?
Featured
 Laser hair removal
Laser hair removalYou can expect permanent results in all but one area. Do you know which one?
 Scar treatment
Scar treatmentIf you want to diminish a noticeable scar, know these 10 things before having laser treatment.
 Botox
BotoxIt can smooth out deep wrinkles and lines, but the results arent permanent. Heres how long botox tends to last.
Featured
 Find a Dermatologist
Find a DermatologistYou can search by location, condition, and procedure to find the dermatologist thats right for you.
 What is a dermatologist?
What is a dermatologist?A dermatologist is a medical doctor who specializes in treating the skin, hair, and nails. Dermatologists care for people of all ages.
Chronic hives
Diagnosis
To diagnose chronic hives, your health care provider will likely talk with you about your symptoms and look at your skin. One of the telling features of chronic hives is that the welts come and go at random. You might be asked to keep a diary to keep track of:
- Your activities
- Any medications, herbal remedies or supplements you take
- What you eat and drink
- Where hives appear and how long it takes a welt to fade and whether it leaves behind a bruise or other mark
- Whether your hives come with painful swelling
You may also need blood tests to determine the cause of your symptoms. An accurate diagnosis will guide your treatment options. If needed to clarify the diagnosis, your doctor might take a skin sample (biopsy) to examine under a microscope.
Treatment
Treatment for chronic hives often starts with nonprescription anti-itch drugs (antihistamines). If these don't help, your health care provider might suggest that you try one or more of these treatments:
Prescription anti-itch drugs. The usual treatment for chronic hives is prescription antihistamine pills that don't make you drowsy. These drugs ease itching, swelling and other allergy symptoms. Daily use of these drugs helps block the symptom-producing release of histamine. Examples include:
- Cetirizine
- Desloratadine (Clarinex)
- Fexofenadine
These medications have few side effects. If the nondrowsy antihistamines don't help you, your health care provider may increase the dose or add another type of antihistamine.
Check with your health care provider before taking any of these medications if you're pregnant or breastfeeding, have a long-term medical condition, or take other medications.
Other medications
If the first-choice drugs don't ease your symptoms, other drugs may help. For example:
- Famotidine (Pepcid AC)
- Montelukast (Singulair)
- Doxepin (Silenor, Zonalon)
- Cimetidine (Tagamet HB)
- Nizatidine (Axid AR)
- Ranitidine (Zantac)
- Omalizumab (Xolair)
For chronic hives that resist these treatments, your health care provider might prescribe a drug that can calm an overactive immune system. Examples are cyclosporine (Gengraf, Neoral, Sandimmune), tacrolimus (Prograf, Protopic, others), hydroxychloroquine (Plaquenil) and mycophenolate (Cellcept, Myfortic).
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Chronic hives can go on for months and years. They can interfere with sleep, work and other activities. The following self-care tips may help you manage your condition:
- Avoid triggers. These can include foods, medications, pollen, pet dander, latex and insect stings. If you think a medication caused your welts, stop using it and contact your primary care provider. Some studies suggest that stress or fatigue can trigger hives.
- Use a nonprescription anti-itch drug. A nonprescription anti-itch (antihistamine) pill that doesn't cause drowsiness may help ease itching. Examples include loratadine (Alavert, Claritin, others) and cetirizine (Zyrtec Allergy).
- Apply cold. Soothe the skin by covering the itchy area with a cold washcloth or rubbing an ice cube over it for a few minutes.
- Take a comfortably cool shower or bath. Some people might relieve itching in the short term by taking a cool shower or bath. Try sprinkling the bath water with baking soda or oatmeal powder (Aveeno, others).
- Apply an anti-itch cream or lotion. Try a cream with menthol for a soothing effect.
- Wear loose, smooth-textured cotton clothing. Avoid wearing clothing that's rough, tight, scratchy or made from wool.
- Protect your skin from the sun. Liberally apply sunscreen about a half hour before going outdoors. When outdoors, seek shade to help relieve discomfort.
- Track your symptoms. Keep a diary of when and where hives occur, what you were doing, what you were eating, and so on. This may help you and your health care provider identify triggers.
Preparing for your appointment
You'll likely start by seeing your primary care provider. Or you may be referred to an allergy specialist or a doctor who specializes in the diagnosis and treatment of skin conditions (dermatologist).
What you can do
Here are some tips to help you get ready for your appointment.
- List your symptoms, when they occurred and how long they lasted.
- List any medications you're taking, including vitamins, herbs and supplements. Even better, take the original bottles and a list of the doses and directions.
- List questions to ask your doctor.
For chronic hives, questions you may want to ask include:
- What is likely causing my symptoms?
- How long will hives last?
- What kinds of tests do I need? Do these tests require any special preparation?
- What treatments are available, and which do you suggest?
- What are the alternatives to the primary approach that you're suggesting?
- Do these treatments have any side effects?
- Do I need prescription medication, or can I use nonprescription drugs to treat the condition?
- Does the medicine you're prescribing have a generic version?
What to expect from your doctor
Your health care provider is likely to ask you a few questions, such as:
- When did you first have symptoms?
- What did your skin reaction look like when it first appeared?
- Have your symptoms changed over time?
- Have you noticed anything that makes your symptoms worse or better?
- Do your skin lesions mainly itch, or do they burn or sting?
- Do your skin lesions go away completely without leaving a bruise or a mark?
- Do you have any known allergies?
- Have you ever had a similar skin reaction before?
- Have you tried a new food for the first time, changed laundry products or adopted a new pet?
- What prescriptions, nonprescription medications and supplements are you taking?
- Have you started taking any new medications or started a new course of a medication you've taken before?
- Has your overall health changed recently? Have you had any fevers or have you lost weight?
- Has anyone else in your family ever had this kind of skin reaction? Do other family members have any known allergies?
- What at-home treatments have you used?
Hives (Urticaria) and Angioedema Overview
Hives (Urticaria) and Angioedema Overview
 Hives or welts, also known as urticaria, are itchy, raised, reddish areas on the skin. About a quarter of the general population can have hives during their life. Hives often appear without warning and may start at any age.Angioedema is swelling below the surface of the skin and fatty tissue. Areas of
Hives or welts, also known as urticaria, are itchy, raised, reddish areas on the skin. About a quarter of the general population can have hives during their life. Hives often appear without warning and may start at any age.Angioedema is swelling below the surface of the skin and fatty tissue. Areas of 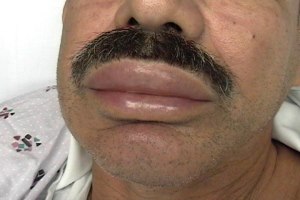 swelling may be painful. Angioedema usually occurs in the face, throat, hands, and feet. Swelling can also occur in the abdomen or other areas of the body. Throat swelling can be life threatening and requires immediate medical attention. It is important to understand that angioedema is a medical term to describe swelling. It can be found with many different disorders. Angioedema can occur with or without hives. There are several different ways swelling can occur. Understanding the underlying mechanism of swelling or the specific disease is critical in determining the best treatment.
swelling may be painful. Angioedema usually occurs in the face, throat, hands, and feet. Swelling can also occur in the abdomen or other areas of the body. Throat swelling can be life threatening and requires immediate medical attention. It is important to understand that angioedema is a medical term to describe swelling. It can be found with many different disorders. Angioedema can occur with or without hives. There are several different ways swelling can occur. Understanding the underlying mechanism of swelling or the specific disease is critical in determining the best treatment.
Hives and Angioedema Symptoms & Diagnosis
Hives are itchy and can occur anywhere on the body including the face, extremities, chest, back or face. Hives range in size from just a few millimeters to several centimeters. An individual hive usually fades within a 24-hour period and the skin returns to normal without leaving any marks or bruising.Doctors will classify your hives based on how long you have had them. This helps doctors think about possible causes of your hives. When hives occur for less than 6 weeks, we call this acute urticaria. When hives last longer than 6 weeks, we change the name to chronic urticaria. Sometimes the hives in chronic urticaria can occur with angioedema (swelling). There are two types of chronic urticaria: spontaneous urticaria, and chronic inducible urticaria. Chronic inducible urticaria is caused by an environmental trigger such as heat, cold, or pressure applied to the skin. The most common form of the inducible urticarias is called dermatographic urticaria. It can occur in all age groups. Dermatographic urticaria is triggered by shearing forces against the skin such as scratching, pressure from tight clothing resulting in the linear appearing hives. Stroking, or scratching the skin with a firm object will elicit the response in 5-7 minutes. Hives can last for 15 minutes to 3 hours. Antihistamines are frequently an effective form of treatment. Spontaneous remission can occur in 2-3 years.Both forms of chronic urticaria are not dangerous. Usually the cause of chronic spontaneous urticaria cannot be identified, but allergy is not typically a cause. This is a constant finding of medical authorities and researchers around the world. The absence of an identifiable trigger can be frustrating for patients.Classifications
Acute | Chronic (spontaneous or inducible) |
Spontaneous hives, angioedema or both for less than 6 weeksOften due to viral infections (most common), food, drug, environmental allergy and insect bites | Spontaneous hives, angioedema or both for more than 6 weeksSpontaneous hives often have an association with autoimmunityInducible urticaria:Physical Urticaria (non-allergic hives from environmental triggers)Scratching/rubbing (dermatagraphic urticaria)Pressure/tight clothes (pressure urticaria)Sweating/increased temperature (cholinergic urticaria)Cold exposure, ice (cold urticaria)Swelling from vibration (vibration induced angioedema)Sunlight (solar urticaria) Water (aquagenic urticaria) |
Modified from http://www.urtikaria.net/en/forms-of-urticaria/overview.html
Angioedema without Urticaria: A Special SituationTalk to your doctor if swelling occurs without hives. This may suggest a special situation requiring additional evaluation. Sometimes high dose antihistamines may not improve your swelling. This is because the mechanism (cause) of swelling may be different than that of hives.Swelling without hives may be due to:1. Aspirin or nonsteroidal anti-inflammatory drug (NSAIDs) such as ibuprofen2. ACE inhibitors (a class of blood pressure medications)The generic names of these medications end in pril such as lisinopril. ACE inhibitors can cause swelling at any time during the course of therapy, even after years of being on the medication. 3. Hereditary angioedema (swelling)Hereditary angioedema (HAE) is a rare genetic disorder in which patients have a defect in the gene that controls a regulatory blood protein called C1 Inhibitor. When C1 Inhibitor does not function properly, fluids can shift out of the blood and into tissues to cause swelling. Antihistamines, corticosteroids and epinephrine will not be effective in treating swelling in patients with HAE, however targeted treatments are available once your diagnosis is established. Over 50% of patients with HAE will have their first swelling episode prior to age 12.4. Acquired angioedemaAcquired angioedema (swelling) is an acquired form of C1 inhibitor deficiency that can occur in certain diseases. This is not hereditary or passed to your children.Angioedema without Urticaria
Spontaneous | Medication induced | Underlying disease |
Unclear causeAutoimmune | Aspirin/NSAID inducedACE inhibitor induced angioedema | Hereditary angioedema (HAE)Acquired angioedema |
Hives and Angioedema Treatment & Management
The goals of treatment are to: Provide relief of itching Make hives more tolerable Provide complete resolution of your hivesMedications will help your itching and reduce hives. Medications will not cure hives but can help to completely resolve them. Antihistamines are the best initial medication to treat your hives. Sometimes, a combination of several antihistamines or an increased dose of one antihistamine may be recommended.Older antihistamines such as Benadryl (sedating antihistamines) may cause you to get sleepy, cause dryness and only last for several hours. Newer non-sedating antihistamines are less likely to make you sleepy. They have fewer side effects and last much longer. Non-sedating antihistamines (shown below) are often the first medication doctors will prescribe for your hives. High dosages, up to 4 times the recommended dose, are often well tolerated and can help control your itching. This will also help to prevent the use of other medications that may have more side effects.About 50% of chronic spontaneous urticaria (hives over 6 weeks with no identifiable cause) will respond to antihistamine as discussed above. For those who do not improve on antihistamines, 65% respond to omalizumab (Ref 2). Omalizumab is an FDA approved treatment of chronic urticaria. This medication is injected under the skin once a month. Corticosteroids, such as prednisone or prednisolone may help hives. These are not an ideal treatment for long-term use but may have a role to relieve severe symptoms for a few days. Your doctor will outline a treatment plan that allows you to increase treatment during an outbreak of hives or swelling and reduce medications when the hives or angioedema are not as bothersome.Chronic hives can last for many years but will often go away. Hives will resolve in half of patients within 1-2 years and 80-90% of patients will improve within 5 years. Even if a patients hives improve, it is not unusual to see the hives recur months to years later.Antihistamines commonly used to treat urticaria:
Sedating antihistamines | Non-sedating antihistamines |
hydroxyzine (Atarax) | cetirizine (Zyrtec) |
diphenhydramine (Benadryl) | levocetirizine (Xyzal) |
fexofenadine (Allegra) | |
loratadine (Claritin) | |
desloratadine (Clarinex) |
References1. Bernstein JA, Lang DM, Khan DA et al. The diagnosis and management of acute and chronic urticaria: 2014 update. J Allergy Clin Immunol. 2014;133:1270-72. Kaplan AP. Therapy of chronic urticaria: a simple, modern approach. Ann Allergy Asthma Immunol. 2014;112:419-253. Zuraw BL, Bernstein JA, Lang DM et al. A focused parameter update: hereditary angioedema, acquired C1 inhibitor deficiency, and angiotensin-converting enzyme inhibitor-associated angioedema. J Allergy Clin Immunol. 2013;131:1491-3Find out more about skin allergies. Test your knowledge and see how much you know about hives.The AAAAI's Find an Allergist / Immunologist service is a trusted resource to help you find a specialist close to home.12/27/2023