Does touching hives make them worse

How to Prevent Scratching When You Have Chronic Hives
Updated on March 13, 2024
Chronic spontaneous urticaria (CSU) is a condition that causes recurring episodes of hives or whealsswollen, raised, itchy welts on the surface of the skin. In addition to hives, some people with CSU also experience angioedema, which is swelling in deeper layers of the skin.
The defining characteristic of CSU is that symptoms appear without any apparent or identifiable or consistent triggerin other words, the cause is unknown. For many people, these symptoms occur every day or nearly every day. For hives to be diagnosed as chronic, symptoms need to last for six weeks or longer. (Hives that last for fewer than six weeks are not considered chronic and are called acute spontaneous urticaria). While six weeks is the minimum, many people experience symptoms for months or years.
While the condition resolves within a few years in many cases, it requires treatment.
The impact of itch
Mentioned above, itching is one of the main symptoms of CSU. Itch can manifest as a stinging, burning, or tickling sensation, or another irritating sensation that causes the desire to scratch.
With CSU, itching can be intense and severe. Itch can be a frustrating and distressing symptom. It can have a significant impact on a persons quality of life, disrupting sleep and many aspects of everyday life.
The importance of avoiding scratching
If you are experiencing itch, its important to avoid scratching as much as possible. Reasons to avoid scratching include:
- Scratching can make itching worse. Scratching causes the release of a substance called histamine, which triggers more itching.
- Scratching can trigger hives. Scratching, rubbing, and pressure on the skin can also trigger hives and angioedema for some people. Usually this is associated with inducible urticaria, but a person can have both inducible and spontaneous urticaria at the same time.
- Scratching can damage the skin. Damaged skin is more susceptible to infections. Damaging the skin can also lead to scars and other skin changes.
Strategies to avoid scratching
Its important that your treatment plan include strategies to reduce itch and prevent scratching. The first and most important strategy is to work with a healthcare provider. Based on your symptoms, your overall health, and other factors, your healthcare provider can prescribe medications to help control hives and itch. A healthcare provider can also help identify any health condition that may be causing or contributing to hives.
Additionally, you can try these strategies to cope with itch without scratching:
- Apply an anti-itch cream. Ask your healthcare provider about over-the-counter medications that can be applied to the skin to help ease itch, such as calamine lotion. Always tell your healthcare provider about any and all medications and over-the-counter medicines you are using.
- Apply moisturizer. Applying moisturizer can help ease itch. Choose fragrance-free moisturizers. Keeping the skin moisturized can also prevent itch by preventing dry skin.
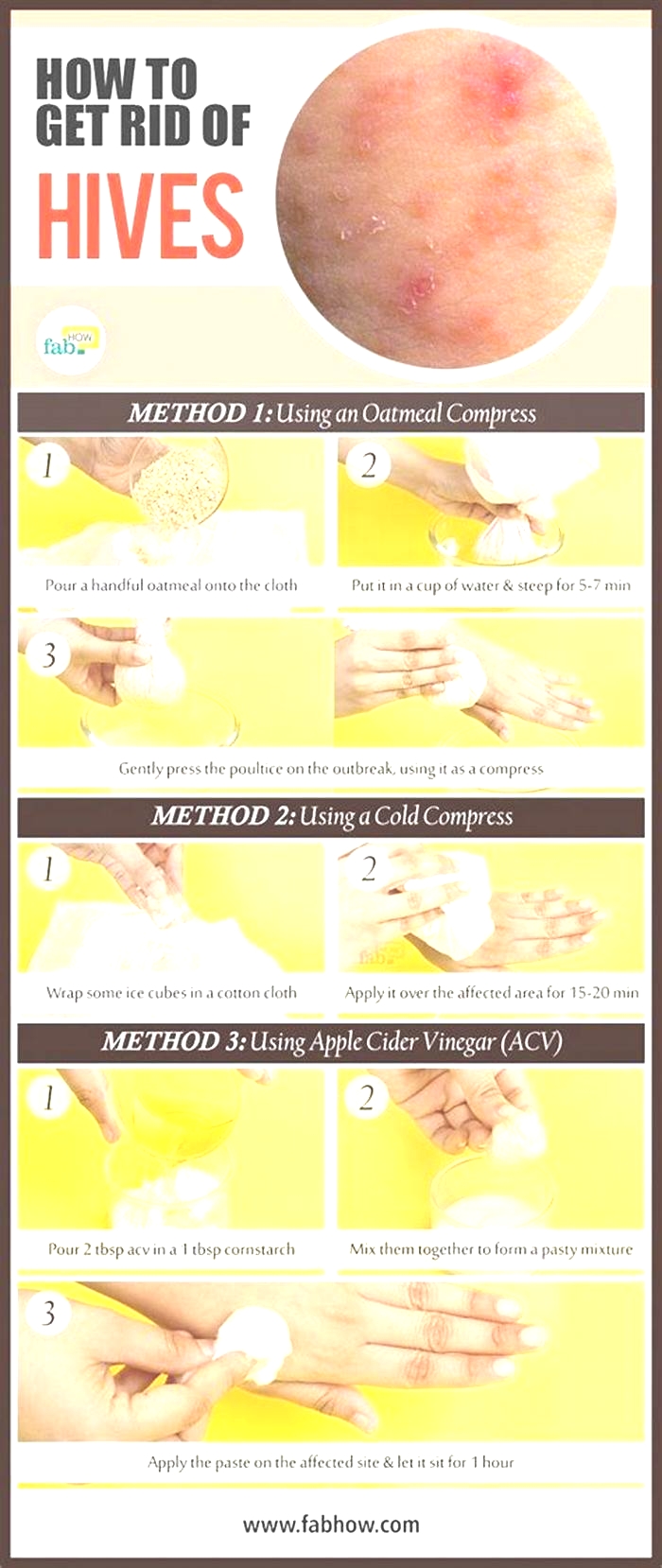
- Apply a cold compress. A cold compress is a clean washcloth soaked in cold water. However, do not do this if exposure to cold induces hives.
- Find distractions. Find ways to keep your hands busy and your mind distracted when you are experiencing itch. Play a game on your phone, knit, fidget with a toy, meditate, read, or watch a show.
- Scratch something else. Some people with conditions that cause itch find it helpful to scratch something besides their skin when they are itchy, such as a patch of Velcro.

Dominique Dabija, Prasanna Tadi, and Gerard N. Danosos. Chronic Urticaria. StatPearls. April 17, 2023.American College of Allergy, Asthma, & Immunology. Chronic Spontaneous/Idiopathic Urticaria (Chronic hives).Thomas M. Ruenger. Hives. Merck Manual Consumer Version. January 2023.Vishakha V. Sinha, Mrunalini Vinay Kalikar, et al. Comparative study of efficacy and safety of cetirizine and bilastine in patients of chronic spontaneous urticaria: Open-label, randomized, parallel-group study. Perspective in Clinical research, 2023. Vol. 13, No. 4.Abhishek De, Kiran Godse, Dhiraj Dhoot, and Aarti Sarda. Real-Life Experience of Efficacy and Safety of Bilastine in the Refractory Cases of Chronic Spontaneous Urticaria and its Effect on the Quality of Life of Patients. Indian Journal of Dermatology, 2021. Vol. 66, No. 2.Yuzhou Huang, Yi Xiao, et al. Association of Chronic Spontaneous Urticaria With Anxiety and Depression in Adolescents: A Mediation Analysis. Frontiers in Psychiatry, 2021. Vol. 12.Mayo Clinic. Itchy skin (pruritus).Takemichi Fukasawa, Asako Yoshizaki-Ogawa, et al. Pharmacotherapy of ItchAntihistamines and Histamine Receptors as G Protein-Coupled Receptors. International Journal of Molecular Sciences, 2022. Vol. 23, No. 12.Iolanda Alen Coutinho, Frederico Soares Regateiro, et al. Refractory chronic urticaria in adults: clinical characterization and predictors of severity. Allergy, Asthma & Clinical Immunology. Vol. 2020. Vol. 16.Elena Kovalkova, Daria Fomina, et al. Comorbid Inducible Urticaria Is Linked to Non-Autoimmune Chronic Spontaneous Urticaria: CURE Insights. Journal of Allergy and Clinical Immunology: In Practice, 2024. Vol. 12, No. 2.Merck Manual Professional Version. Description of Skin Lesions.American Academy of Dermatology Association. 10 Ways To Get Relief From Chronic Hives.Merck Manual Professional Version. Urticaria.American Academy of Dermatology Association. Hives: Self-Care.National Organization for Rare Disorders. Urticaria, Cold.
9 Ways to Ease the Itch of Chronic Hives
They're itchy, red, and raised and often appear at the worst possible times. About 20 percent of the population will get them at least once in their lives, according to the American College of Allergy, Asthma & Immunology. They're hives. And hives that last more than six weeks are considered chronic (persistent or recurring). For some people, these hives are a result of allergies, but for others there's no discernible cause. Chronic hives with no known cause are called chronic idiopathic urticaria (hives).
The itching associated with these hives, which stems from the release of natural chemicals called histamines by your bodys immune system, can dramatically affect your quality of life. This is among the main findings of a study published in August 2015 in the journal Annals of Allergy, Asthma & Immunology. Still, there's a lot you can do to ease the itch of chronic hives.
Hives (Urticaria)
What are hives?
Hives, or urticaria, are flat red welts that can appear anywhere on the skin and usually itch. Hives often occur as an allergic reaction to something eaten or something that has contacted the skin. Foods, medicines, and plants are common causes, but sun exposure, stress, infections, and autoimmune diseases have also been known to cause hives.
Symptoms include an itchy, stinging pink rash of slightly swollen skin. The rash may wax and wane in severity. Acute hives typically resolve within six weeks, but chronic hives (urticaria) can persist for months or years.
Hives often resolve on their own, especially in children. Otherwise, treatment for acute hives involves oral antihistamine medications to help relieve the itching and stinging. Chronic hives that do not improve with antihistamines may be treated additionally with corticosteroids, antibiotics, and other stronger medicines. A study found that 35% of people with chronic hives, are symptom free within one year, with another 29% having some reduction of symptoms.
You can safely treat this condition on your own as long as you does not develop trouble breathing. Any antihistamine (like Zyrtec, Clarinex, etc) works.
11 Habits That Make Acne Worse
Blame it on the hormones or genetics, sometimes acne can be entirely out of your control. And, of course, no one likes to have these tiny disruptions on the skin.
You might be investing in a ton of skincare products to keep these tiny zests at bay, but do you know that certain lifestyle habits can make your acne worse? Here are ten bad habits that can worsen your acne problem.
What Our Experts Say
Touching your face constantly, especially when suffering from acne, is a big no.
- Prajkta Sapre, PG, Cosmetic Technology, Product Development Executive, SkinKraft
Highlighting the importance of why one should avoid touching the face, Prajkta Sapre, Product Development Executive, SkinKraft, says, Touching your face constantly, especially when suffering from acne is a big no. Our fingertips are a source of vast microbial flora which may be harmful.
She adds that touching acne repeatedly contributes in spreading the P. acnes bacteria, which is responsible for the acne and its inflammation. Squeezing and popping pimples, acne, and blackheads makes it worse.
Prajkta recommends that three basic habits need to be followed to reduce acne. These are,
1. Maintaining good body hydration and a healthy diet.
2. Cleansing your face according to your skin type.
3. Exfoliating your face with chemical exfoliators carefully according to the skin type.
11 Habits That Make Acne Worse
1. Constantly Popping The Breakouts
Most people tend to pop the breakouts, but remember, whenever you pop acne, you push some of the content of the acne inside. This could be pus, bacteria, or dead skin cells. This can flare up the infection, leading to more acne, along with scars and pain.
Instead, no matter how strong the urge to pop or squeeze acne is, stop yourself from touching it. You can apply acne medication or consult a dermatologist if it is too troublesome.

2. Rubbing Sweat During Workouts
While working out, you might be using a towel to constantly rub your face and wipe out the drips of sweat. But do you know that constant rubbing of the face can irritate the skin, leading to breakouts?
Instead, avoid rubbing your face and pat the sweat dry. Always use a clean and soft towel.
3. Constantly Scrubbing Your Skin
If you think that constant scrubbing can stop acne, then know that regular scrubbing can irritate the skin. This can flare up and cause further infection. [1]
Instead, use a mild non-comedogenic cleanser to clean your face. Use your fingertips to gently clean the face in a circular motion, rinse with warm water, and pat dry with a soft clean towel.

4. Wash Your Face Throughout The Day
It is a common misconception that washing your face throughout the day will keep the acne away. While it is essential to keep the skin clean, frequent washing can irritate your skin. This can lead to more frequent breakouts.
Instead, wash your face twice a day, once when you wake up in the morning and once when youre about to go to bed. However, if you have done a workout, applied makeup, or are sweating in general, wash your face to keep it clean.
Did You Know?
Acne is the eighth most prevalent disease in the world. An estimated 9.4% global population is affected by acne. [2]
5. Using Makeup That Clogs Pores
If you're using makeup or any skin/hair care products that can clog the skin pores, stop using them immediately. If you continue to use them, they may clog the pores and cause further breakouts.
Instead, switch to better makeup and skincare products. Remember to read the labels. Any products that have the word non-comedogenic are safe to use.
6. Changing Your Acne Cream Frequently
Many are often desperate to get rid of acne, and tend to try various new acne creams available in the market. But, know that switching creams too frequently can irritate your already sensitive skin. Plus, a product takes time to work.
Instead of frequently changing your acne cream, use a product for at least 3-4 months to see whether it's working or not. If not, switch to another product. However, always consult a dermatologist before applying any acne cream or switching products.
7. Sharing Makeup & Makeup Applicators
While acne is not contagious, when you use other peoples applicators or makeup, the acne bacteria, oil, and dead cells from the other persons skin can land up on your skin. This can clog your skin pores, causing acne and blemishes.
Instead of using other peoples products, always use only your makeup and makeup applicator.
8. Not Cleansing Your Makeup
Any makeup can clog the pores if you wear it for a long time.
Instead, make it a point to wash your face and cleanse makeup with a good cleanser before going to bed.
9. Applying Acne Creams Only On Blemishes
Most people make the mistake of applying creams only on the blemishes they can see. But that doesn't stop new breakouts from popping up.
Instead, remember to apply your acne medication evenly over your skin, especially in breakout areas like the jawline, forehead, and nose.
10. Not Cleaning Your Phone Screen
Not cleaning your phone screen can worsen your acne condition. The unclean screen has a lot of bacteria, and pressing it against the skin can lead to breakouts.
Instead, remember to clean your phone screen regularly or try using headphones.
11. Sleeping On Dirty Pillows
Dirty pillows can cause eyelash mites[3]. Apart from that, dirty pillow cases may also increase the risk of developing acne in people prone to breakouts. If you don't change your pillowcase frequently, dead cells, bacteria, and oil can pile up quickly, leading to acne breakouts.
Instead, remember to change your pillowcase every 7-10 days.

SkinKraft Tip:
Spot application of tea tree oil can keep your acne breakout at bay. A research study revealed that a 5% tea tree oil gel was more effective at reducing acne than a placebo.
How To Develop Good Skin Habits?
1. Avoid eating refined carbohydrates like pasta, bread, crackers, and say yes to whole grains. A research study found that people who consumed added sugar more frequently had a 30% greater risk of developing acne and those who ate pastries regularly had a 20% greater risk.
2. Let your skin heal naturally, just keep it clean by using gentle soap and lukewarm water.
3. When youre already going through a bout of breakout, your skin remains sensitive. So, avoid going out into the sun as the harmful sun rays can cause further damage to your skin.
Wrapping Up
Your lifestyle habits can impact your acne condition to a great extent. While certain habits can worsen the condition, following a healthy lifestyle and skincare habits can help you control your acne breakouts and reduce your visits to your dermatologist. However, if your acne problems persist, do not hesitate to ask your dermatologist for advice.
Note:
If youre still unable to control your acne breakouts even after following these tips, do see a dermatologist.
Begin By Knowing Your Skin