How long do hives last on a dog

Dog Hives (Urticaria | welts): Causes, Diagnosis & Treatment
What Are Dog Hives (Urticaria)?
Hives, otherwise known as urticaria by medical professionals, are one abnormality you may see. They occur when your dog is allergic to something, such as an insect, medication, or food. Recognizing hives in dogs and understanding the cause is essential to relieving your dogs discomfort and preventing dog hives in the future.
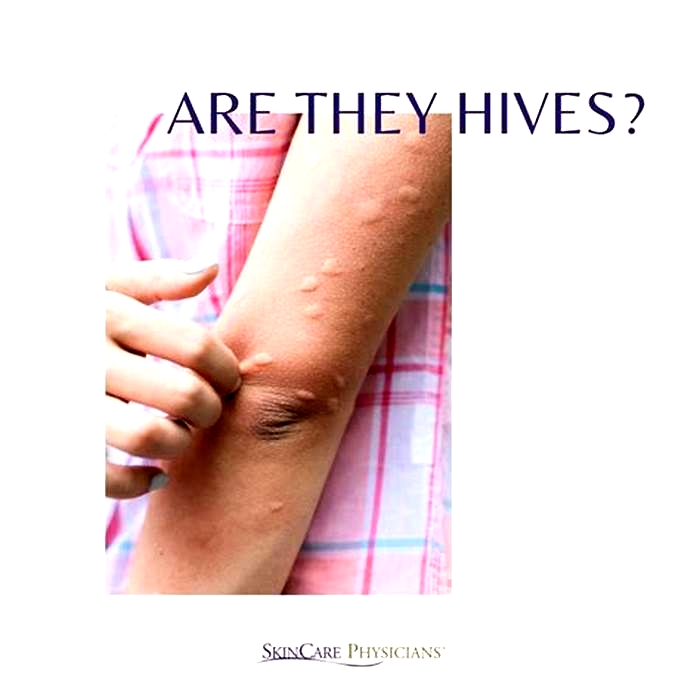
What do dog hives look like?
- Dog hives look like raised bumps on the skin, usually about the size of a nickel.
- Hives are usually red in color; however, you may not notice redness if they are on a very furry part of your dog. In this case, your pets hives may only look like fur-covered bumps. Sometimes, its difficult to see the raised bumps, and you may only feel them when petting your dog.
- Dog hives can appear anywhere on the body, including the face, tongue, neck, legs, chest, abdomen, or back. They can affect just one area of the body or the entire body.
- Dog hives are very itchy. This may be the first thing you notice before seeing or feeling hives on your dogs skin. Your dog will likely be trying to scratch, lick, or bite the areas affected as it will be itchy.
- Hives usually happen very fast within minutes after exposure to whatever caused them.
- You may notice excessive drooling and a swollen/puffy face if the hives affect your dogs throat or mouth.
What causes hives on a dog?
Dog hives are almost always related to exposure to an allergen. Once exposed to an allergen, mast cells in your dogs body release a substance called histamine. Histamine causes blood vessels to dilate, which leads to raised welts on your dogs skin.
The most common allergens causing dog hives include:
- Insect bite or sting, or ingesting an insect (photo recommendation: dog playing with bee)
- Vaccinations
- Acute allergic reactions to medications (chemotherapy, vitamin K, antibiotics)
- Food allergies
- Environmental allergies (grasses, trees, mold, dust mites, etc.)
- Contact allergens such as shampoos, insecticides, cleaning products
- Ingesting or skin exposure to toxic plants
Much less common causes of hives in dogs include prolonged exposure to extreme temperatures (hot or cold), strenuous exercise, parasites, or significant psychological stress.
Insect bites/stings, food, and medications are the most common causes of hives in dogs.
How are dog hives diagnosed?
As a pet parent, it can be worrisome to see these skin rashes, but luckily, for your vet to diagnose your dogs hives. Your vet will use a combination of your history and their physical examination findings.
Its essential to think about anything new your dog may have been exposed to. Did you see them playing with a bee? Were they recently vaccinated? Did they start a new medication or a new food? During the physical exam, your veterinarian will look at your dogs skin to evaluate hives and where the hives are located.
If your veterinarian is having trouble diagnosing your dogs hives or the reason for their hives, they may perform additional diagnostics, such as blood work, skin cytology, skin scrapings, or fecal analysis.
How to treat & get rid of dog hives?
Treatment for hives in dogs can be simple or more extensive, depending on the cause, severity, and duration of the allergic reaction.
To get your dog quick relief from the swelling and itchiness related to hives, your veterinarian will usually administer an injection of diphenhydramine (an antihistamine) and a corticosteroid. Once your dog is feeling better and discharged from the hospital, your veterinarian may also recommend that you continue giving your dog Benadryl two to three times a day at home for a couple of days.
To prevent hives from reoccurring, you need to understand what caused them in the first place so that you can avoid the allergen in the future. If there is no apparent cause for your dogs hives (such as insect bite, medication, or vaccinations), it may be more challenging to understand how to prevent hives in the future. Environmental and dietary allergies are two possible causes of hives that may require further diagnostics and treatment.
Environmental allergies
If your dog has recurrent hives or has other signs of allergies, your veterinarian may recommend testing for environmental allergies with serum allergy testing or intradermal allergy testing. With these results, your veterinarian can create a plan to desensitize your dog to these allergies with allergen-specific immunotherapy.
If you determine that you cannot eliminate the allergens in your dogs environment or pursue allergen-specific immunotherapy treatment, your veterinarian may recommend:
- Giving your dog daily antihistamines (such as Benadryl, zyrtec, or hydroxyzine)
- Giving your dog other prescription-strength allergy medications such as apoquel or cytopoint
- Starting daily skin health supplements, such as omega-three fatty acids.
- Frequently bathing your dog with medicated high-quality shampoo
Food allergies
Allergies that stem from food can also cause recurrent episodes of hives in dogs. The most common cause of allergies in dogs include chicken, beef, dairy, and egg 2. Recurrent episodes of hives can also be related to dietary allergies. To diagnose a food allergy, your veterinarian may recommend a diet trial for 6-8 weeks with a prescription food or an over-the-counter diet with a different protein source, like fish or venison. If your dog responds positively to a food trial, you can continue the special diet long term.
Are dog hives dangerous?
Dog hives are rarely life-threatening. However, there are a few less common situations where hives can affect your dogs breathing and become dangerous.
- Hives in the face, neck, or throat can cause severe swelling that impacts breathing, which can become life-threatening.
- The presence of hives anywhere may indicate your dog is having or about to have an anaphylactic reaction, which causes constriction of airways and difficulty breathing. 3 Besides hives, other signs of anaphylaxis include vomiting, diarrhea, facial swelling, drooling, blue gum color, and collapse.
If you notice that your dog has hives, pay particular attention to how they are breathing and for any other concerning changes in their behavior. If you are concerned your dog may be having severe allergic reactions, take them to the emergency room immediately to rule out a medical emergency.
At-home remedies for dog hives
If possible, take your dog to the veterinarian if you notice they have hives, especially if this is a first-time problem. If your dog chronically or intermittently has hives and the issue has previously been discussed with a veterinarian, some at-home remedies may help relieve the allergic reaction.
- If the hives are not affecting your dogs face, neck, throat, or ability to swallow, you can administer Benadryl by mouth. Always discuss if this is appropriate for your dog with your veterinarian first and receive instructions about dosage and frequency.
- If the hives were caused by a contact allergen (such as grasses/trees or chemicals) or insect bites you can help relieve itchiness by bathing with a gentle oatmeal-based dog shampoo can help your dog feel more comfortable.
- Apply a cold compress to the hives or the most severely affected areas of your dogs skin. Be careful never to apply a cold compress for more than 10 minutes at one time, and always wrap the ice or cold object in a towel before applying it to your dogs skin.
How long can hives last?
Hives can appear and disappear quickly, with each hive only lasting around 23 hours. However, depending on the cause, they may reappear and continue affecting someone for days, weeks, or longer.
People can have acute hives, which occurs due to a specific trigger and resolves within
This article looks at how long hives last, factors that influence their duration, and treatment.
Each hive lasts only
Acute hives appear quickly and do not last long. Doctors classify hives as acute if the overall duration is less than 6 weeks.
However, around 25% of people go on to develop chronic hives. This is when hives regularly reappear over 6 weeks or more.
For many individuals, chronic hives eventually clear on their own, but this can take months. According to the American Academy of Dermatology Association (AAD), around half of people with chronic hives spontaneously recover within 1 year.
Acute hives often occur in response to an allergen or irritant. When the immune system perceives a substance as a threat, it releases histamine and other chemicals. This causes tiny blood vessels under someones skin to leak fluid, which accumulates and causes the bump.
Some
- food allergens, such as milk, eggs, tree nuts, peanuts, or shellfish
- contact allergens, such as latex or animal dander
- insect bites or stings
- medications
Any drug can cause hives, but some of the medications most commonly associated with this symptom include:
Acute hives can also occur in response to viral infections, parasitic infections, or during times of stress.
According to a 2018 review, doctors are unsure of the cause of acute hives in
Chronic hives may have the same cause as acute hives, but with symptoms lasting longer than 6 weeks. However, chronic hives are often not due to an allergen and instead have a physical cause.
There are two subcategories of chronic hives: inducible urticaria and chronic idiopathic urticaria.
Chronic idiopathic hives
Chronic idiopathic urticaria has no clear cause and is the most common form of chronic hives. Researchers are working to understand why this type of hives occurs, but a leading theory links it with autoimmunity.
Autoimmunity occurs when a persons immune system mistakenly attacks healthy tissue, and several autoimmune conditions are associated with chronic hives. The most common is thyroid disease, which is present in
This suggests that the hives may result from someones immune system not functioning as it should. Other conditions that can occur alongside chronic hives include type 1 diabetes, lupus, and rheumatoid arthritis.
Infections can also be associated with the onset of chronic hives. This includes bacterial, viral, and parasitic infections. Again, this may result from autoimmunity an infection may trigger a change in how the persons immune system works.
Inducible hives
Inducible or physical urticaria is less common than chronic idiopathic urticaria. With this subtype, it is possible to purposely induce the hives by a person exposing their skin to certain triggers, which could include:
- Scratching or pressure: The
most common type of inducible hives is known as dermatographia. This condition involves developing hives as a response to scratching or drawing on the skin. - Cold: Cold hives occur on someones skin or mouth after exposure to cold temperatures. Triggers include consuming iced drinks, touching cold water, or going outside in cold weather.
- Heat: Cholinergic hives occurs when an individuals body becomes hot or sweaty. Hot baths, exercise, and spicy food can be triggers.
- UV light: Solar hives occur in response to UV light from the sun and certain light bulbs, such as those in tanning beds.
- Water: Some people develop hives if their skin comes into contact with water. This is known as aquagenic urticaria and is very rare.
Doctors diagnose hives by performing a physical examination. There is no test to determine whether the persons hives are acute or chronic, so they will use the length of time they recur to do this.
The doctor may also ask an individual:
- when the rash began
- the shape, size, and distribution of the rash
- where on the body they first noticed the rash
- if they have had any insect bites
- if they live or work with common hive triggers, such as chemicals, animals, or latex gloves
- if they have bone or joint pain, fever, or abdominal pain
- if anyone in their family experiences hives
- if they take any medications or supplements
The doctor may use a skin prick test and serum-specific IgE test to check if the acute hives result from a specific substance, such as food, dust mites, or chemicals. Alternatively, they may refer someone to an allergy clinic for these tests.
However, in cases of chronic hives, allergy testing is rarely useful. A doctor may check for other underlying health conditions by performing additional tests, such as:
The most suitable treatment depends on whether the person has acute hives or chronic hives.
Acute hives
Doctors typically recommend second-generation antihistamines as the first-line treatment for acute hives, such as:
- loratadine (Claritin)
- desloratadine (Clarinex)
- fexofenadine (Allegra)
- cetirizine (Zyrtec)
- levocetirizine (Xyzal)
They may prescribe a standard dose or increase by up to 4 times if the individual does not respond.
If these medications do not improve symptoms, the doctor may recommend an additional antihistamine, such as cimetidine (Tagamet), famotidine (Pepcid), or ranitidine (Zantac). They may recommend a 310-day course of corticosteroids to help control the symptoms in severe cases.
The doctor may prescribe an epinephrine auto-injector if they think the individual is at risk of anaphylaxis, which is a severe allergic reaction that restricts breathing. This provides emergency medicine to treat anaphylaxis quickly.
The doctor will then reassess the individual in 26 weeks.
Chronic hives
Doctors may recommend a four-step treatment plan for chronic hives. This approach involves using an antihistamine daily, which may be up to 4 times the regular dosage depending on how the individual responds.If necessary, they may prescribe a second antihistamine or another medication, such as montelukast (Singulair). With persistent hives, they may suggest a high potency antihistamine, such as hydroxyzine or doxepin.
The final step is for a doctor to refer the individual to a specialist for immunomodulatory therapy. This may involve taking medications such as omalizumab (Xolair) or cyclosporine (Sandimmune).
Once symptoms are under control, a doctor may gradually reduce the dosage of these medications. If the hives have an identifiable cause, such as cold or heat exposure, adopting changes to avoid the triggers wherever possible is also important.
The AAD suggests the following methods for people to reduce irritation and itchiness in hives:
- applying topical anti-itch medications, such as calamine lotion
- wearing loose-fitting clothing
- moisturizing with fragrance-free lotion to prevent dry skin
- using cold compresses several times per day
However, it is important for individuals to try to determine whether the hives have a specific trigger, in addition to relieving symptoms. If someone has cold hives, for example, a cold compress may make them worse.
Therefore, it is a good idea for people to keep a symptom diary, recording when the hives occur and any factors that might have contributed. Symptom diaries are also useful to refer to at medical appointments. A person can take note of:
- the date and time the hives appear
- what they were doing just before they developed
- what they have had to eat or drink
If any common factors emerge when the hives occur, a person can try to temporarily avoid these to see if it helps. It is important for people to do this with the guidance of a doctor, allergist, or dietitian if someone has food-related hives.
Learn more about remedies and treatments for hives here.
Hives do not last long, taking only 23 hours to fade. However, more can appear, which makes the symptoms last longer. Acute hives can develop and resolve on their own within 6 weeks, while chronic hives can last much longer.
Doctors treat acute and chronic hives differently, so it is advisable for people to speak with a medical professional about this symptom, especially if the hives last longer than 6 weeks.
If hives or swelling occur in the mouth and airways, making it difficult to breathe, dial 911 or the number of the nearest emergency department immediately.