How many days does rabies take effect in humans
Rabies
Rabies the word probably brings to mind an enraged animal frothing at the mouth. This painful, life threatening, and preventable condition can result from an encounter with an infected animal.
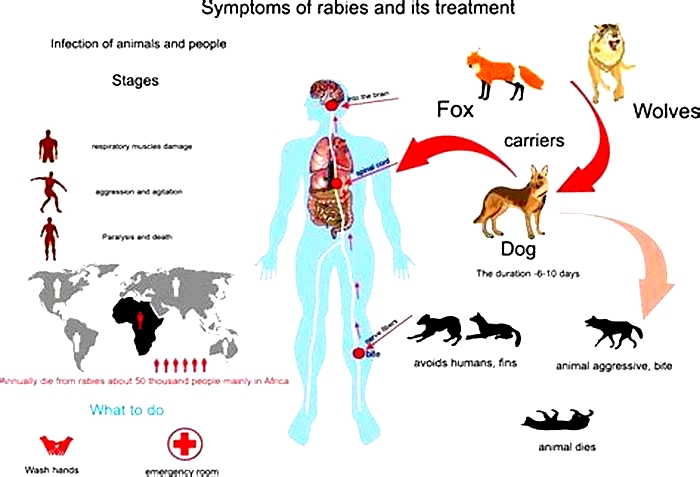
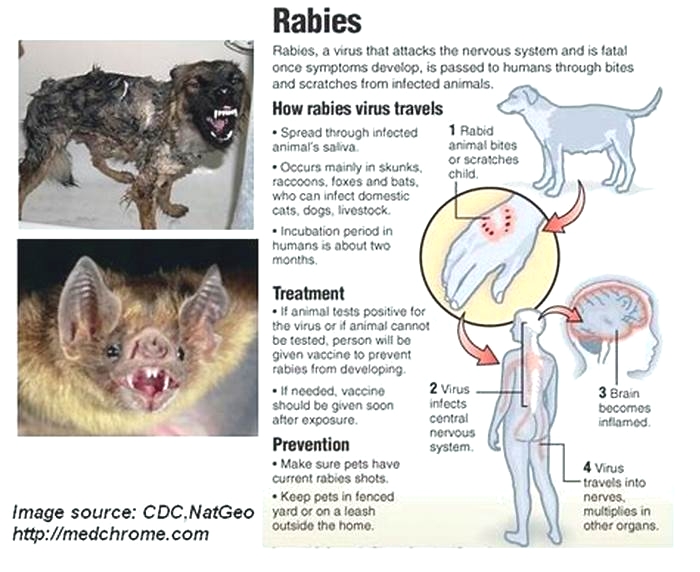
Rabies is caused by a virus that affects the central nervous system (CNS), in particular the brain.
Domestic dogs, cats, and rabbits and wild animals such as skunks, raccoons, and bats are able to transfer the virus to humans via bites and scratches. The key to fighting the virus is a quick response.
According to the
The availability of vaccines for both animals and humans has led to a steep decline in rabies cases in the United States. The country has
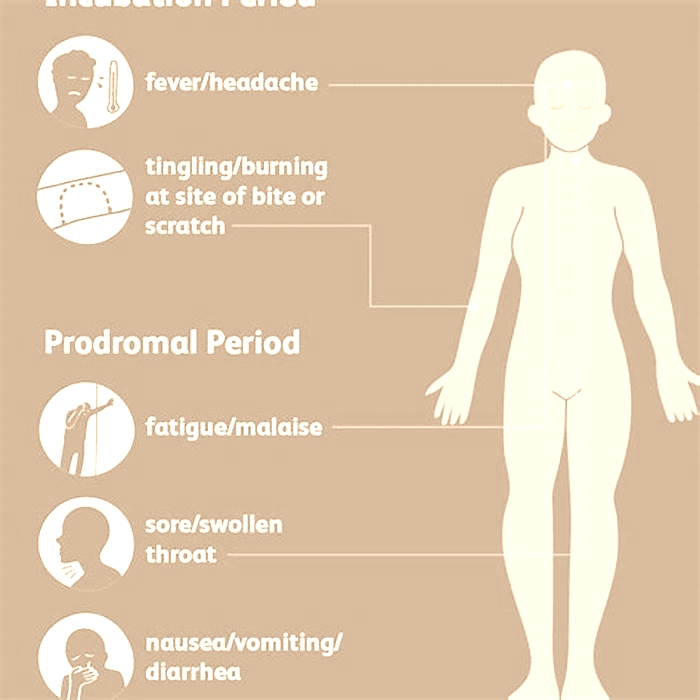
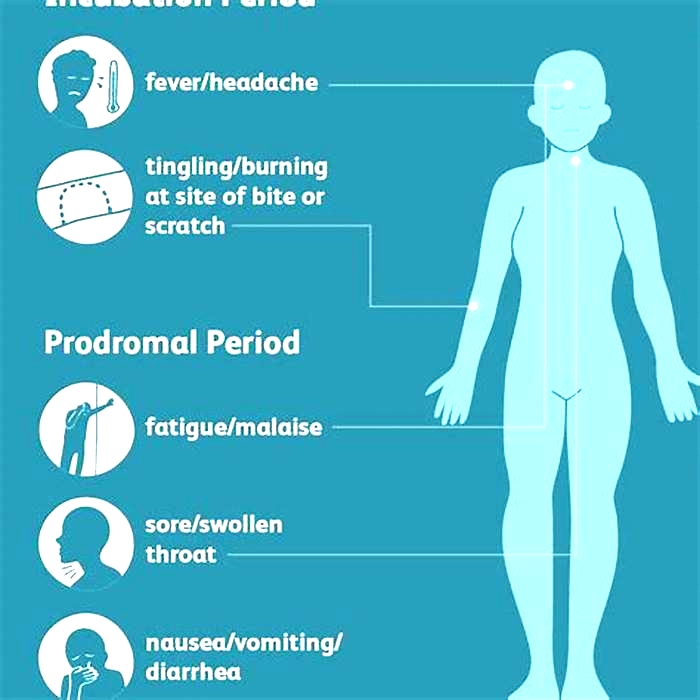
The period between the bite and the onset of symptoms is called the incubation period. It usually takes
The initial onset of rabies begins with flu-like symptoms, including fever, muscle weakness, and tingling. You may also feel burning at the bite site.
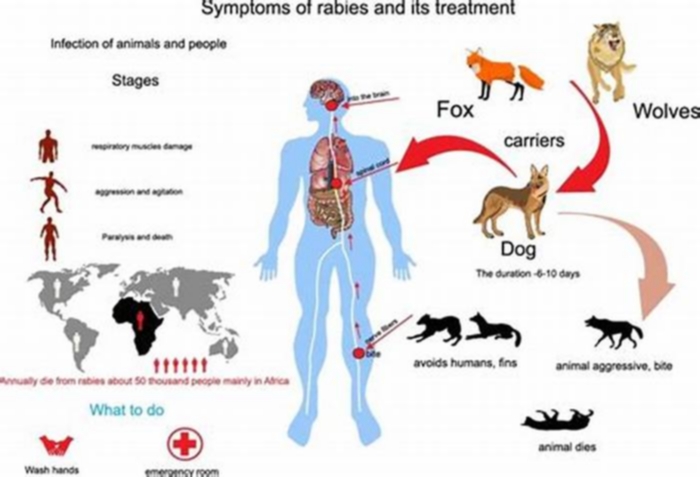
As the virus continues to attack the CNS, there are two different types of the disease that can develop: furious rabies and paralytic rabies.
Furious rabies
People who develop furious rabies will be hyperactive and excitable and may display erratic behavior. Other symptoms include:
Paralytic rabies
This form of rabies takes longer to set in. People with the infection slowly become paralyzed, will eventually slip into a coma, and die. According to the WHO,
Animals with rabies transfer the virus to other animals and humans via a scratch or saliva following a bite. However, any contact with the mucous membranes or an open wound can also transmit the virus.
The transmission of this virus is considered to occur exclusively from animal to animal and animal to human. While human-to-human transmission of the virus is extremely rare, there have been a handful of cases reported following corneal transplants. For humans who contract rabies, a bite from an unvaccinated dog is by far the most common culprit.
Once a person has been bitten, the virus spreads through their nerves to their brain. Bites or scratches on the head and neck are thought to speed up the brain and spinal cord involvement because of the location of the initial trauma. For that reason, if youre bitten on the neck, its especially important to seek help immediately.
Following a bite, the rabies virus spreads by way of the nerve cells to the brain. Once in the brain, the virus multiplies rapidly. This activity causes severe inflammation of the brain and spinal cord after which the person deteriorates rapidly and dies.
Animals that can spread rabies
Both wild and domesticated animals can spread the rabies virus. The following animals are the main sources of rabies infection in humans:
- dogs
- bats
- ferrets
- cats
- cows
- goats
- horses
- rabbits
- beavers
- coyotes
- foxes
- monkeys
- raccoons
- skunks
- woodchucks
For most people, the risk of contracting rabies is relatively low. However, there are certain situations that may put you at a higher risk. These include:
- living in an area populated by bats
- living in a rural area where theres greater exposure to wild animals and little or no access to vaccines and preventive therapy
- traveling to developing countries
- frequent camping and exposure to wild animals
- being under the age of 15 years old (rabies is most common in this age group)
Although dogs are responsible for most rabies cases worldwide, bats are the cause of most rabies deaths in the United States.
Theres no test to detect the early stages of rabies infection. After the onset of symptoms, a doctor can use tests such as a blood, tissue, or saliva test to help determine whether you have the disease. Tissue tests include the direct fluorescent antibody (DFA) test and a biopsy of the neck.
If youve been bitten by a wild animal, a doctor will typically administer a preventive shot of the rabies vaccine to stop the infection before symptoms set in.
Once a person has developed rabies, its rare for the disease to be cured. However, after being exposed to the rabies virus, you can have a series of injections to prevent an infection from setting in.
Rabies immunoglobulin, which gives you an immediate dose of rabies antibodies to fight the infection, helps to prevent the virus from getting a foothold. Then, getting the rabies vaccine is the key to avoiding the disease.
Animal control will probably try to find the animal that bit you so that it can be tested for rabies. If the animal isnt rabid, you can avoid the large round of rabies shots. However, if the animal cant be found, the safest course of action is to take the preventive shots.
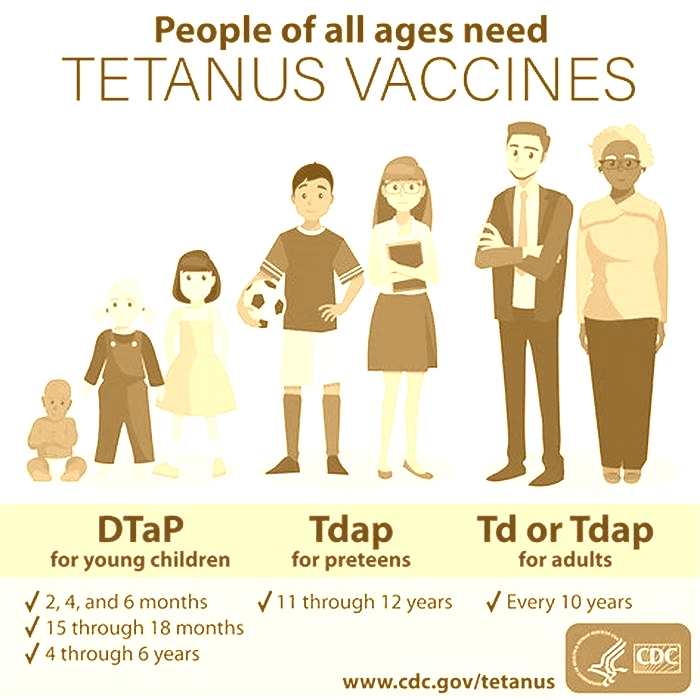
Getting a rabies vaccination as soon as possible after an animal bite is the best way to prevent the infection. The rabies vaccine is given in a series of five shots over 14 days.
Doctors will treat your wound by washing it for at least 15 minutes with soap and water, detergent, or iodine. Then, theyll give you a shot of the rabies immunoglobin and youll start the round of four injections for the rabies vaccine. This protocol is known as post-exposure prophylaxis.
Side effects of the rabies vaccine
The rabies immunoglobulin and vaccine can rarely cause side effects, including:
Rabies is a preventable disease. There are simple measures you can take to help keep you from catching rabies:
- Get a rabies vaccination before traveling to developing countries, working closely with animals, or working in a lab handling the rabies virus.
- Vaccinate your pets.
- Keep your pets from roaming outside.
- Report stray animals to animal control.
- Avoid contact with wild animals.
- Prevent bats from entering living spaces or other structures near your home.
Report any signs of an infected animal to your local animal control or health departments.
What are the signs and symptoms of rabies?
After a rabies exposure, the rabies virus has to travel to the brain before it can cause symptoms. This time between exposure and appearance of symptoms is the incubation period. It may last for weeks to months.The incubation period may vary based on
- the location of the exposure site (how far away it is from the brain),
- the type of rabies virus, and
- any existing immunity.
The first symptoms of rabies may be similar to the flu, including weakness or discomfort, fever, or headache. There also may be discomfort, prickling, or an itching sensation at the site of the bite. These symptoms may last for days.
Symptoms then progress to cerebral dysfunction, anxiety, confusion, and agitation. As the disease progresses, the person may experience delirium, abnormal behavior, hallucinations, hydrophobia (fear of water), and insomnia. The acute period of disease typically ends after 2 to 10 days. Once clinical signs of rabies appear, the disease is nearly always fatal, and treatment is typically supportive. Less than 20 cases of human survival from clinical rabies have been documented. Only a few survivors had no history of pre- or postexposure prophylaxis.
The signs, symptoms, and outcome of rabies in animals can vary. Symptoms in animals are often similar to those in humans. These include early nonspecific symptoms, acute neurologic symptoms, and ultimately death.
Everything You Ever Wanted to Know About the Rabies Vaccine
Rabies only rarely affects humans in the United States. But for people who do contract the virus, its almost always fatal without prompt medical care.
This serious virus, which is typically transmitted via animal bites and scratches, attacks the central nervous system, explains William R. Dodge, MD, an emergency medicine physician with Providence Mission Hospital in Mission Viejo, California.
Once the virus reaches your brain, it causes neurological symptoms, like confusion, hallucinations, and seizures, followed by coma and eventually death.
Thats why youll want to contact a doctor right away if youve received a bite or scratch from a wild animal or unvaccinated pet, Dodge says, even if you arent sure they have rabies.
Heres the good news: The rabies vaccine can protect you from the virus. But youll typically get this vaccine after exposure to the virus, unlike preventive vaccines that you get before potentially contracting a condition.
Below, find answers to seven commonly asked questions about the rabies vaccine, including why its so important and how to tell when you need it.
Getting a rabies vaccine immediately after a bite from an animal that might have rabies can jumpstart your bodys fight against the virus, Dodge says.
The rabies vaccine triggers your immune system to produce antibodies, Dodge explains. These special proteins can recognize foreign invaders, like viruses, and destroy them.
The rabies vaccine may prevent you from getting the virus if you receive it as soon as possible ideally within 1 to 2 days of exposure.
The incubation period for the rabies virus typically ranges from a few days to several months. During the incubation period, you wont experience symptoms because the virus has yet to reach your brain. Once the virus reaches your brain and symptoms develop, the vaccine can no longer offer protection.
FYIAdults and older children will receive the rabies vaccine in the shoulder muscle, while younger children and babies will receive injections in the thigh muscle.
Your pets might get a yearly rabies booster or one every few years. But humans often need multiple injections for full protection.
The number of doses youll need depends on two things: whether youve had a rabies vaccine in the past and the type of exposure youre receiving treatment for.
Its essential to get medical attention as soon as possible after a bite from an animal that could have rabies, even if youve recently had a rabies vaccine booster, Dodge emphasizes.
Depending on your risk of coming into contact with a rabid animal in the future, your doctor might recommend getting another booster within 3 years after your first two doses, Dodge says.
The most common side effects of the rabies vaccine include:
- pain at the injection site
- skin discoloration
- swelling
- induration, or hardening or thickening of the skin at the injection site
These mild, local reactions typically go away within a few days. You can usually treat them with over-the-counter medications like ibuprofen or acetaminophen.
You might also experience:
If you experience any of these symptoms, Dodge advises contacting your doctor. They can monitor your symptoms and offer more guidance on options for relief.
Keep in mind that if you may have been exposed to rabies, youll need to get the vaccine even if youre immunocompromised, pregnant, breastfeeding or chestfeeding, or have existing health conditions. This is because rabies is almost always fatal.
Before getting vaccinated, let your doctor know if youve ever had an allergic reaction to a vaccine. They can monitor you for signs of an allergic reaction after you receive the rabies vaccine.
Unlike most other vaccines, you typically only receive the rabies vaccine after youve had exposure or potential exposure to the virus. You may also choose to get the vaccine if you plan to travel to countries where rabies is endemic, or regularly found.
Any mammal can carry rabies, including both wild animals and unvaccinated pets, such as:
- bats
- raccoons
- skunks
- squirrels
- foxes
- dogs
- coyotes
- cats
- ferrets
The virus lives in saliva and brain and nervous system tissue. So an animal with rabies doesnt have to bite you to transmit the virus. You could contract the virus from a scratch, or even a lick.
If you have any doubts about an animals vaccine status, you should assume it may have rabies and contact your doctor immediately if the animal:
- scratches you, even if the scratch doesnt bleed
- nibbles uncovered skin
- bites you, even if it doesnt bleed
- licks your skin
Maybe you came into contact with an animal that could have rabies, but dont know for sure if the animal bit you. For example, you might wake up to find a bat in your bedroom. In this case, you should assume it bit you and call your doctor or head to the emergency room immediately.
Youll typically only receive a preventive rabies vaccine if you:
- work with or frequently come in contact with animals examples include veterinarians, animal control officers, and animal quarantine facility staff
- plan to spend a month or longer in an area of the world where rabies is common
- plan to participate in activities that may expose you to rabid animals, like hiking in the wilderness, in areas where rabies is common
The rabies vaccine does not provide lifelong protection. Protection can last for anywhere from 6 months to 2 years, depending on how many doses youve had.
For example, if you get two doses of the rabies vaccine as a preventive measure, youll need a booster dose in 2 years if you still have a high risk of exposure to rabies.
If you get all four doses of the vaccine after exposure to rabies, youll need the vaccine again if youre exposed to the virus again.
The out-of-pocket cost of the rabies vaccine ranges from about
When medically necessary after a bite from a stray dog or wild squirrel, for instance health insurance will usually cover the vaccine.
Your health insurance provider may not cover preventive vaccines given before exposure. Those are generally considered elective rather than medically necessary.
If you think you may have been exposed to rabies, your best option is to head to your nearest emergency room (ER).
Many primary care and urgent care clinics dont administer this vaccine. So, if you make an appointment with your regular doctor and they recommend a rabies vaccine, theyll typically send you to the ER anyway.
If you want to get the vaccine as a preventive measure, you can make an appointment at some pharmacies, including certain CVS and Walgreens locations.
Thanks to widespread animal vaccination, rabies has significantly declined in the United States. But if you do happen to encounter an unvaccinated or wild animal, a postexposure rabies vaccine can save your life.
When administered in time, the rabies vaccine can help your immune system fight off the virus effectively. The sooner you get it after exposure, the greater your chances of protecting yourself.
Always contact your doctor immediately after receiving a scratch or bite from an animal if you dont know its vaccination status.
Rebecca Strong is a Boston-based freelance writer covering health and wellness, fitness, food, lifestyle, and beauty. Her work has also appeared in Insider, Bustle, StyleCaster, Eat This Not That, AskMen, and Elite Daily.