Is hives a serious allergic reaction

Anaphylaxis
The immune system produces antibodies that defend against foreign substances. This is good when a foreign substance is harmful, such as certain bacteria or viruses. But some people's immune systems overreact to substances that don't normally cause an allergic reaction.
Allergy symptoms aren't usually life-threatening, but a severe allergic reaction can lead to anaphylaxis. Even if you or your child has had only a mild anaphylactic reaction in the past, there's a risk of more severe anaphylaxis after another exposure to the allergy-causing substance.
The most common anaphylaxis triggers in children are food allergies, such as to peanuts and tree nuts, fish, shellfish, wheat, soy, sesame and milk. Besides allergy to peanuts, nuts, fish, sesame and shellfish, anaphylaxis triggers in adults include:
- Certain medications, including antibiotics, aspirin and other pain relievers available without a prescription, and the intravenous (IV) contrast used in some imaging tests
- Stings from bees, yellow jackets, wasps, hornets and fire ants
- Latex
Although not common, some people develop anaphylaxis from aerobic exercise, such as jogging, or even less intense physical activity, such as walking. Eating certain foods before exercise or exercising when the weather is hot, cold or humid also have been linked to anaphylaxis in some people. Talk with your health care provider about precautions to take when exercising.
If you don't know what triggers an allergy attack, certain tests can help identify the allergen. In some cases, the cause of anaphylaxis is not identified (idiopathic anaphylaxis).
Allergic Reactions after COVID-19 Vaccination
A severe allergic reaction can cause:
- difficulty breathing or wheezing,
- a drop in blood pressure,
- swelling of the tongue or throat, or
- a generalized rash or hives, which may include mucus membranes.
If You Had a Severe Allergic Reaction to a COVID-19 Vaccine in the Past
If you had a severe allergic reaction after receiving a particular type of COVID-19 vaccine (either mRNA or Novavax), you should not get another dose of that type of vaccine. You will likely be able to receive the alternate vaccine type. Your doctor may refer you to an allergy and immunology specialist for additional care or advice.
Types of COVID-19 vaccines:
If You Had a Non-severe Allergic Reaction to a COVID-19 Vaccine in the Past
If you had an allergic reaction to a COVID-19 vaccine that started within 4 hours of getting vaccinated, but the reaction was not considered severe by a medical professional, you likely can receive another dose of the same type of COVID-19 vaccine under certain conditions, such as being observed in the clinic for 30 minutes after vaccination. Your doctor may refer you to an allergy and immunology specialist for additional care or advice.
If You Have Had an Allergic Reaction to Other Vaccines, Injectables, Medications
In most cases, you will likely be able to receive a COVID-19 vaccine. All allergies should be discussed with your doctor or vaccine provider before receiving a vaccine.
- If you had a severe allergic reaction to an ingredient used in one type of COVID-19 vaccine, you may be able to get the other type of COVID-19 vaccine.
- If you had a non-severe allergic reaction to an ingredient used in the COVID-19 vaccine, your doctor may still recommend being vaccinated under certain conditions.
Your doctor is your best source of information if you might have an allergy to an ingredient thats used in COVID-19 vaccines. Your doctor may refer you to an allergy and immunology specialist for additional care or advice.
If You Had a Rash on the Arm Where You Got a COVID-19 Shot
If you had a red, itchy, swollen, or painful rash where you got a COVID-19 shot, you should still get another shot at the scheduled date and time. This applies to the updated (20232024 formula) COVID-19 vaccine.
These rashes can start a few days to more than a week after your shot and are sometimes quite large. These rashes are also known as COVID arm. Tell your vaccination provider that you experienced a rash or COVID arm after your previous shot. Your vaccination provider may recommend that you get your next COVID-19 vaccine in the opposite arm if possible.
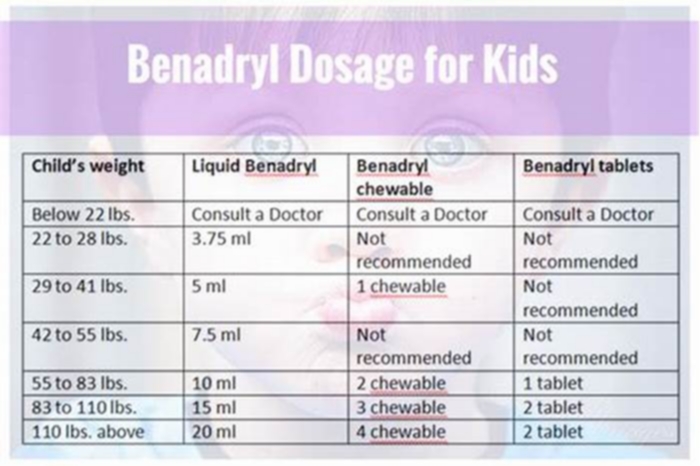
If the rash is itchy, you can take an antihistamine. If it is painful, you can take a pain medication like acetaminophen or a non-steroidal anti-inflammatory drug (NSAID).
Safeguards Are in Place
- Everyone who gets a COVID-19 vaccine may be monitored onsite for at least 15 minutes after vaccination.
- Some people may bemonitored for 30 minutes after vaccination including in the following situations:
- You had an immediate (within 4 hours) allergic reaction that was not severe from a previous dose of that type of COVID-19 vaccine.
- Youve had a non-severe allergic reaction to an ingredient used in the COVID-19 vaccine.
CDC Is Monitoring Reports of Severe Allergic Reactions
If someone has a severe allergic reaction after getting vaccinated, their vaccination provider may send a report to theVaccine Adverse Event Reporting System (VAERS).VAERS is a national system that collects reports from healthcare professionals, vaccine manufacturers, and the public about adverse events that happen after vaccination. Reports of adverse events that are unexpected, appear to happen more often than expected, or have unusual patterns are followed up with specific studies.
Learn more about how CDC and federal partners are monitoring the safety of COVID-19 vaccines in the United States, including reports of selected adverse events after COVID-19 vaccination.
Hives and angioedema
Overview
Hives
Hives
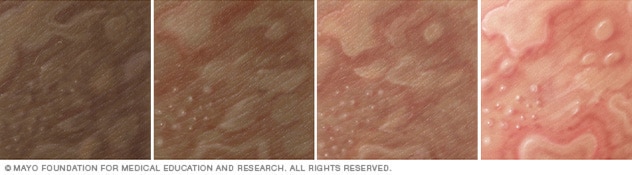
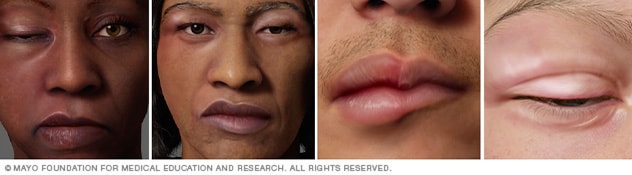
Illustration of hives on different skin colors. Hives can cause swollen, itchy welts. Hives is also called urticaria.
Angioedema
Angioedema
Illustration of angioedema on different skin colors. Angioedema causes swelling in the deeper layers of skin, often of the face and lips. It often goes away within a day.
Hives also known as urticaria (ur-tih-KAR-e-uh) is a skin reaction that causes itchy welts that range in size from small spots to large blotches. Hives can be triggered by many situations and substances, including certain foods and medications.
Angioedema can arise with hives or alone. It causes swelling in the deeper layers of skin, often around the face and lips. Short-lived (acute) hives and angioedema are common. Most times, they are harmless, clear up within in a day and don't leave any lasting marks, even without treatment. Hives that last longer than six weeks are called chronic hives.
Hives and angioedema are usually treated with antihistamine medication. Angioedema can be life-threatening if swelling of the tongue or in the throat blocks the airway.
Symptoms
Hives
The welts associated with hives can be:
- Skin-colored, reddish on white skin, or purplish on black and brown skin
- Itchy, ranging from mild to intense
- Round, oval or worm-shaped
- As small as a pea or as large as a dinner plate
Most hives appear quickly and go away within 24 hours. This is known as acute hives. Chronic hives can last for months or years.
Angioedema
Angioedema is a reaction similar to hives that affects deeper layers of the skin. It can appear with hives or alone. Signs and symptoms include:
- Welts that form in minutes to hours
- Swelling, especially around the eyes, cheeks or lips
- Mild pain and warmth in the affected areas
When to see a doctor
You can usually treat mild cases of hives or angioedema at home. See your health care provider if your symptoms continue for more than a few days.
If you think your hives or angioedema was caused by a known allergy to food or a medication, your symptoms may be an early sign of an anaphylactic reaction. Seek emergency care if you feel your tongue, lips, mouth or throat swelling or if you're having trouble breathing.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
ErrorEmail field is required
ErrorInclude a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Causes
For most people who experience acute hives and angioedema, the exact cause can't be identified. The conditions are sometimes caused by:
- Foods. Many foods can trigger reactions in people with sensitivities. Shellfish, fish, peanuts, tree nuts, soy, eggs and milk are frequent offenders.
- Medications. Many medications may cause hives or angioedema, including penicillins, aspirin, ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve) and blood pressure medications.
- Airborne allergens. Pollen and other allergens that you breathe in can trigger hives, sometimes accompanied by upper and lower respiratory tract symptoms.
- Insect bites and infections. Other causes of acute hives and angioedema are insect bites and infections.
Risk factors
Hives and angioedema are common. You may be at increased risk of hives and angioedema if you:
- Have had hives or angioedema before
- Have had other allergic reactions
- Have a family history of hives, angioedema or hereditary angioedema
Complications
Severe angioedema can be life-threatening if swelling of the tongue or in the throat blocks the airway.
Prevention
To lower your likelihood of experiencing hives or angioedema, take the following precautions:
- Avoid known triggers. If you know what has triggered your hives, try to avoid that substance.
- Bathe and change your clothes. If pollen or animal contact has triggered your hives in the past, take a bath or shower and change your clothes if you're exposed to pollen or animals.
Oct. 27, 2023
Overview of Allergic Reactions
Allergen immunotherapy, usually allergy shots (injections), can be given to desensitize people to the allergen when some allergens, especially airborne allergens, cannot be avoided and the drugs used to treat allergic reactions are ineffective.
With allergen immunotherapy, allergic reactions can be prevented or reduced in number and/or severity. However, allergen immunotherapy is not always effective. Some people and some allergies tend to respond better than others.
Immunotherapy is used most often for allergies to
When people are allergic to unavoidable allergens, such as insect venom, immunotherapy helps prevent anaphylactic reactions. Sometimes it is used for allergies to animal dander, but such treatment is unlikely to be useful. Immunotherapy for peanut allergy is available, and immunotherapy for other food allergies is being studied.
Immunotherapy is not used when the allergen, such as penicillin and other drugs, can be avoided. However, if people need to take a drug that they are allergic to, immunotherapy, closely monitored by a doctor, can be done to desensitize them.
In immunotherapy, tiny amounts of the allergen are either injected under the skin or given by mouth, depending on the specific allergen. The first dose is so small that even an allergic person does not react to it. However, the small dose starts to get the person's immune system used to the allergen. Then the dose is gradually increased. Each increase is so small that the immune system still does not react. The dose is increased until the person is not reacting to the same amount of allergen that once caused symptoms. This dose is their maintenance dose. A gradual increase is necessary because exposure to too much allergen too soon can cause an allergic reaction. Injections are usually given once or twice a week until the maintenance dose is reached. Then injections are usually given every 2 to 4 weeks. The procedure is most effective when maintenance injections are continued throughout the year, even for seasonal allergies.
Alternatively, doses of the allergen may be placed under the tongue (sublingual) and held there for a few minutes, then swallowed. The dose is gradually increased, as for injections. The sublingual technique is relatively new, and how often the dose should be given has not been established. It ranges from every day to 3 times a week. Extracts for grass pollen, ragweed, or house dust mite, placed under the tongue, can be used to help prevent allergic rhinitis.
Immunotherapy for peanut allergy may also be given by mouth. The person receives the first several doses of the allergen over the course of a single day while in a doctor's office or clinic. The person then takes the allergen at home. Each time the dose is increased, the first dose of the higher dosage is given under a doctor's supervision.
Allergen immunotherapy may take 3 years to complete. People who develop allergies again may need another longer course (sometimes 5 years or more) of immunotherapy.