What happens if I give my dog too much Benadryl
A Guide to Handling Accidental Double Doses of Benadryl in Dogs
Hey there, pet parents! Today, were diving into a situation that might have you barking up the worry tree: what to do if youve accidentally given your furry friend a double dose of Benadryl. Before you howl in despair, lets fetch some critical answers and paws-itively useful tips to navigate this hairy situation.
What Just Happened? Understanding the Oopsie
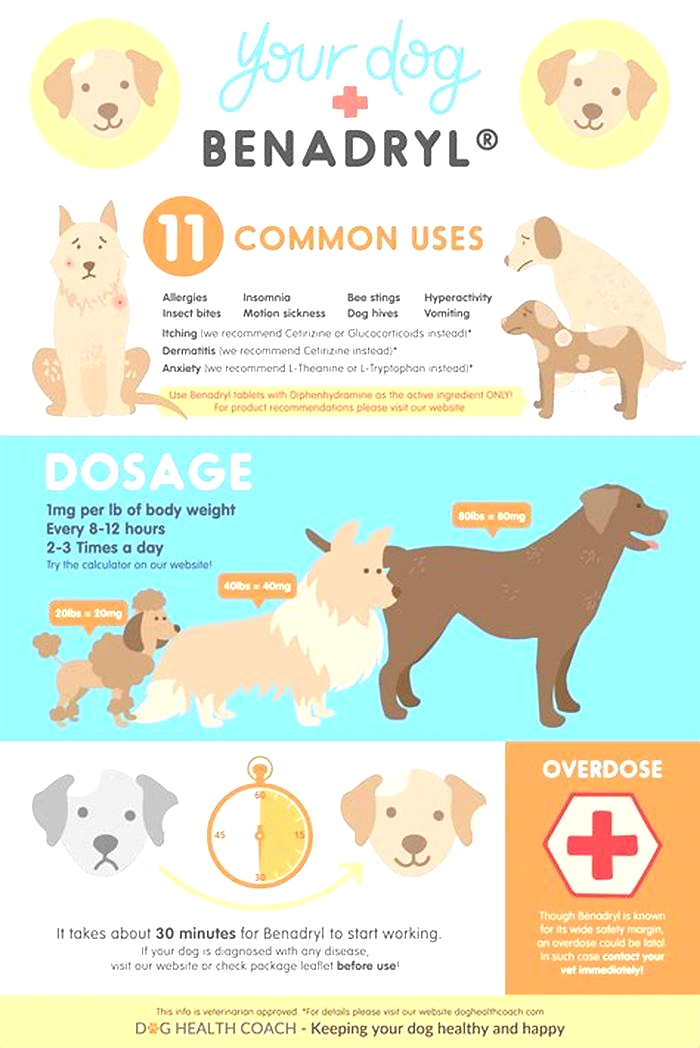
First things first, lets decode what Benadryl (Diphenhydramine) is all about. Its an antihistamine commonly used to relieve symptoms of allergy, hay fever, and the common cold. But did you know its also a go-to for quelling your pups allergic reactions? Thats right, but like all medicines, it comes with a handle with care label.
The Double Dose Dilemma: Charting the Oopsie
| Scenario | Action Steps | Vet Alert? |
|---|---|---|
| Minor Overdose | Monitor closely, offer water, keep calm. | Maybe |
| Moderate Overdose | Induce vomiting if recently ingested, hydrate, observe. | Yes |
| Major Overdose | Immediate vet visit, expect supportive care. | Absolutely |
Bark for Help: When to Call the Vet
Immediate Signs to Watch For: Excessive drooling, rapid breathing, dilated pupils, agitation, or any unusual behavior should have you on the phone with your vet quicker than a Greyhound on a racetrack.
Timing is Everything: If you catch the double dose within 30 minutes, your vet might advise you to induce vomiting under their guidance. Beyond that window, the focus shifts to supportive care and monitoring.
Canine Care 101: Navigating the Next Steps
Stay Cool, Calm, and Collected: Your pooch looks up to you. Showing them that everything is under control (even if youre internally screaming) helps keep their stress levels down.
Hydration Station: Ensure your dog has access to plenty of water. This helps to dilute the medications concentration and supports the bodys natural detox processes.
Food for Thought: Depending on your vets advice, you might need to adjust their diet temporarily. A bland diet can be easier on their stomach during this time.
Comfort is Key: Keep your furry friend in a quiet, comfortable space where they can rest and recover without too much stimulation.
Wrapping It Up with a Bow(wow)
Accidentally doubling up on your dogs Benadryl dose can feel like a nightmare, but with the right knowledge and swift action, it doesnt have to escalate into a full-blown catastrophe. Remember, when in doubt, shout (for your vet, that is). Theyre your best ally in ensuring your pups tail keeps wagging happily.
We hope this guide has shed some light on what to do in this tricky situation. Your journey as a pet parent is filled with learning curves, and its okay to make mistakes as long as you handle them with love and care. Now go forth, armed with knowledge, and continue being the awesome pet parent we know you are!
Interviewer: Dr. Pawsome, first off, thank you for joining us. Lets jump straight in. Whats the very first thing a pet owner should do upon realizing theyve given their dog a double dose of Benadryl?
Dr. Pawsome: Absolutely, happy to be here. When a pet parent realizes the slip-up, the initial step is to remain composed. Panic doesnt help you or your dog. Assess how your dog is currently responding. Are they showing any immediate adverse reactions? If its within that golden half-hour window, a quick call to your vet can guide you on whether inducing vomiting at home is advisable. The key here is quick, calm action.
Interviewer: Thats reassuring to hear. Can you explain why the reaction to a double dose varies so much between dogs?
Dr. Pawsome: Of course, its a great question. Just like humans, every dogs body metabolizes medication differently. Factors like age, weight, pre-existing health conditions, and even breed can influence how a dog reacts to a medication like Benadryl. A robust Great Dane might shrug off a dose that could seriously affect a tiny Chihuahua. Thats why veterinary guidance is so crucial; theyll consider all these factors in their advice.
Interviewer: Speaking of reactions, what are some less obvious signs of an overdose that pet parents might overlook?
Dr. Pawsome: Subtle signs can sometimes provide the earliest warnings of an issue. Beyond the more dramatic symptoms, keep an eye out for things like excessive fatigue, mild confusion, or slight changes in appetite. These symptoms can be easy to miss but might indicate the medication is affecting your pet more than anticipated.
Interviewer: With those potential dangers, what preventative measures can owners take to avoid this situation altogether?
Dr. Pawsome: Prevention is always better than cure, right? A solid approach is double-checking the dosage before administering it. If multiple people are involved in your dogs care, communicate clearly who is responsible for medication times. Technology can also be a great allysetting reminders on your phone or using a dedicated pet care app can prevent double dosing.
Interviewer: If a dog does experience an overdose, how does that affect their long-term health?
Dr. Pawsome: In most cases, with prompt and appropriate care, a single accidental overdose shouldnt have long-term health implications. The liver and kidneys do a fantastic job of processing and eliminating Diphenhydramine. However, repeated incidents or a severe initial overdose could potentially cause longer-term issues, emphasizing the importance of careful dosage and quick action in case of mistakes.
Interviewer: Lastly, for our pet-loving readers, any final words of wisdom from your years of veterinary experience?
Dr. Pawsome: Absolutely. Loving a pet means embracing both joy and responsibility. Mistakes happen, but its how we respond that defines the care we provide. Never hesitate to reach out to your vet, even for what might seem like small concerns. Your vigilance and dedication are what keep your furry family members safe and healthy. Remember, in the world of pet care, no question is too small, and being informed is your greatest tool.
Interviewer: Dr. Pawsome, thank you for sharing your invaluable insights with us today. Heres to safe and happy pets everywhere!
Dr. Pawsome: It was my pleasure. Thank you for spreading awareness on such an important topic. Cheers to all the pet parents out there doing their best every day!
HELP US PUT FOOD ON THE TABLE
What do I do if I gave my dog too much Benadryl? Heres What to Expect
What Are the Side Effects of a Benadryl Overdose in Dogs?
Even at the appropriate dose, some cats and dogs may have what is known as paradoxical excitement. This can lead to excessive excitement, anxiety, and/or aggression, rather than the more common side effect of sedation. This is certainly not the desired outcome, especially if you are hoping Benadryl will keep your dog calmer during a road trip!
Aggression and agitation can also be a symptom of Benadryl overdose. Other potential side effects include:
Some dogs may also have difficulty urinating. These symptoms will usually show up within the first hour of dosing.
In rare cases, Benadryl toxicity can result in death.
Symptoms of Benadryl Poisoning in Dogs
Although Benadryl is generally safe for dogs, some side effects can occur. Side effects usually occur within an hour of administration. They are typically mild and can include:
Overdoses of Benadryl are more often caused by your animal getting a box of the medication from the garbage or medicine cabinet than by being given too much. If you see these signs of an overdose, contact your veterinarian immediately.
Types
Along with a version of diphenhydramine by the name of Vetadryl developed specifically for cats and dogs, there are a few other first generation antihistamines that can be used for dogs. These can include:
Chlorpheniramine This antihistamine is frequently used in small animal veterinary practice and is less likely to cause drowsiness than some of the others
Clemastine Clemastine is classified as an antipruritic (anti-itch), as well as a sedating antihistamine, and is tends to exhibit fewer side effects
Hydroxyzine This drug is a more aggressive antihistamine, but also has more potent side effects
Meclizine Commonly used to reduce nausea, particularly nausea caused by motion sickness
What if I dont have Benadryl? Are there alternatives?
If your dog has allergies and you dont have any Benadryl at home, you can also use cetirizine (Zyrtec) or loratadine (Claritin). As usual, always check with a vet first before administering any human medications to your dog. Especially if your dog has preexisting conditions or is on other medication.
Natural allergy relief can be gained by using quercetin which is a natural ingredient derived from the peels of fruits and vegetables. Not only does quercetin contain antihistamine properties, but it contains anti-inflammatory and antioxidant properties. Chat to your vet about quercetin as an allergy reliever in dogs.
CBD (cannabidiol) is another natural alternative to Benadryl. Its derived from hemp plants and contains absolutely no psychoactive properties so theres no chance of getting your dog high. The benefits of CBD include the relief of skin conditions, as well as itching and hives related to allergies. Dogs that experience motion sickness will also benefit from CBD, as will those suffering from anxiety, pain, or nausea.
Weve all been there. Our sweet, darling pooch looks unwell. We panic. We Google symptoms only to receive confusing advice and very little helpful information. We bribe our unwilling pet into its carrier and rush to the vet. Here, we have to wait for 20 minutes in a crowded waiting room filled with strange sounds and smells that serve only to stress out our already unwell fur-baby.
We endure all of that only to be told that Fluffy has gas. Was it worth all of that stress and expense for such a simple diagnosis? But what is the alternative? You wouldnt want to ignore anything that is potentially serious or leave your sweet pup to suffer needlessly.
We get it, it can be costly to run to the vet for the slightest sniffle or upset. We also know that its stressful finding a vet open late at night, hightailing it across town, and paying exorbitant after-hours consultation fees. This is why its now possible for you to have a vet in your pocket 24/7.
Did you know that 60% of vet visits could have just been a chat? Instead of spending sometimes well over $120 on a visit to the vet, sign up for Online Vet from Petcube for just $19 a month and have unlimited access to a trained vet at any time of day or night, from absolutely anywhere.
Get professional help from a team of certified veterinarians for a fraction of the cost of a normal vet visit. Online vets are available at any time to answer your questions, allay your concerns, and give you back your peace of mind.
The benefits of using this service are more than just financial. Youll be saving plenty of time on a commute and sitting in the waiting room. Add to that, your pet wont need to undergo any unnecessary stress and anxiety of being wrestled into a carrier and taken to the vet if it can be avoided.
You can send text chats as well as photos and videos to help your online vet to better help your floof. And all the information is stored on your pets digital profile, making it super easy for any of our online vets to see your poochs previous history.
While our online vets cant make an official diagnosis or prescribe any medication, they can help you decide whether a vets visit is needed and give you excellent, professional advice and guidance at the click of a button.
Most human medication should never be given to dogs, with the exception of a small number of medications, including Benadryl.
Always make sure to consult with your vet before giving your dog Benadryl to ensure its the right solution for your pet and to ensure youre giving the correct and appropriate dose.
While Benadryl makes a handy fallback plan in an emergency, if your dog suffers from frequent allergies or regularly experiences anxiety, its better to get to the source of the problem instead of relying on Benadryl to deal only with the symptoms. Share this Article


Benadryl For Dogs? Dr. Dan Explains
We report a fatal diphenhydramine poisoning of a 10-year-old, male poodle-cross dog with pre-existing conditions and suspected co-ingestion of ethanol. This case illustrates that diphenhydramine overdose can be fatal in certain circumstances and that analytical toxicology may play an important role in animal death investigations.
Empoisonnement mortel la diphenhydramine chez un chien. Nous signalons un empoisonnement mortel la diphenhydramine chez un caniche crois mle g de 10 ans ayant des conditions prexistantes et une co-ingestion souponne dthanol. Ce cas illustre quune surdose de diphenhydramine peut tre mortelle dans certaines circonstances et quune toxicologie analytique peut jouer un rle important dans les enqutes sur la mort danimaux.
Poisoning of animals with chemical agents is commonplace. Establishing whether the poisoning event was malicious, however, is difficult. In part, this is because of the vast number and types of chemical agents that may be employed. In addition, there is difficulty in discerning between ease of accessibility to the offending agent (i.e., in accidental poisonings) and intentional introduction of those agents to the animals environment (i.e., intentional poisoning). Most poisonings occur within a narrow range of chemical agents, including anticoagulant rodenticides, ethylene glycol, organophosphate and carbamate insecticides, strychnine, and caffeine and other methylxanthines (1). Accidental exposure to these agents results from unbridled roaming, indiscriminate oral evaluation of the environment, and access to human food and supplements. Intentional poisonings differ in that the poison is purposefully introduced into the animals environment, out of the normal context in which the substance resides. Examples include food bowls tainted with ethylene glycol and hot dogs or meat patties contaminated with restricted use pesticides or drugs.
Companion animal poisonings have also been reported to involve household products and drugs for veterinary and human use (2). Medications, whether over-the-counter (OTC) or prescribed, contribute to companion animal fatalities; however, these poisoning events often result from accidental exposure due to ease of accessibility and lack of adequate supervision (3). There may be instances, though, whereby an owner symptomatically treats a pet with their own medication if they think the animal is unwell or in pain (e.g., paracetamol, ibuprofen, or naproxen), thus leading to an unintended consequence. Drugs, or other chemical agents, that are intentionally introduced to animals are commonly supplied in the context of a meal, treat, or drink to reduce texture and palatability inhibitions. Intentional intoxication has also been reported with secondhand cannabis smoke blown into the face of small animals as an adolescent prank (4,5). We report a multi-disciplinary, multi-institutional forensic approach to the intoxication of a dog of advanced age with diphenhydramine, with examination of the underlying question of malicious intent.
The body of a 10-year-old, male poodle-cross dog, weighing approximately 18 kg was submitted to the Animal Health Centre in Abbottsford, British Columbia, for necropsy. The animal was found by police in its residence lying dead adjacent to its deceased owner. The owner had died from blunt force trauma; however, there was no outward evidence of trauma to the dog. Instead, there were 3 empty bottles of sleep aid discovered at the scene. Two bottles were over-the-counter sleep aids containing the active ingredient diphenhydramine. The third bottle was prescription-based, containing the active ingredient Ran-Zopiclone.
The dog was presented dead and frozen. There was moderate decomposition. The animal was well-muscled and there were abundant subcutaneous and visceral fat stores. Along the dorsolateral aspect of the torso and within the inguinal regions, fat lobules featured superficial hemorrhage. The heart was markedly enlarged with circumferential thickening of the left ventricular free wall and at the base, there was a prominent indentation. The right ventricular free wall was moderately dilated and turgid. The lungs were collapsed (atelectatic) and mottled dark red to black. Moderate amounts of dark red frothy fluid filled the tracheobronchial tree. The stomach was markedly distended with partially digested dog food pellets and fetid gas, and there was a moderate amount of partially digested food within the small and large intestines. Throughout the stomach and intestines, the serosa was variegated pale to dark red. There were no other significant gross internal or external lesions. Postmortem X-rays did not reveal any indication of trauma.
There was no indication of infection or inflammation in the examined tissues. Aerobic culture of select internal viscera yielded light to heavy mixed growth of Streptococcus spp. and Enterobacter cloacae, which were likely due to postmortem invasion and bacterial overgrowth rather than representing primary pathogens. Polymerase chain reaction of pooled tissues also proved negative for canine distemper virus (6) and canine parvovirus (7).
Consequently, stomach contents were submitted for toxicology screening. A general organic compound screen by gas chromatography coupled with mass spectral analysis (8,9) was positive for diphenhydramine, but not Ran-Zopiclone. Diphenhydramine was semi-quantitatively estimated at 250 ppm. Additionally, fatty acid ethyl esters (FAEE) were observed suggesting the concomitant ingestion of ethanol and, presumptively, an intentional introduction of the medication to the dog in the context of feed mixed with alcohol. Blood samples to assess circulating concentrations of diphenhydramine, ethanol, and fatty acid ethyl esters were unavailable since the dog was presented in rigor mortis. No other tissue samples were made available for analysis.
Initially, the cause of death for this dog was presumptively attributed to dilated cardiomyopathy. Moreover, periglomerular fibrosis in the kidney, bridging fibrosis in the liver, coronary arteriosclerosis, and parathyroid hyperplasia were sufficiently severe to have contributed to ante-mortem morbidity. Both OTC sleep aids discovered near the body of the dog contained 50 mg of active ingredient diphenhydramine per tablet with 20 tablets dispensed per bottle. All 40 tablets were missing, suggesting the potential for consumption of a maximum dose equivalent to 111 mg/kg body weight (BW). Based on this observation, analytical toxicology was performed and confirmed the presence of diphenhydramine in the stomach contents ( ) in sufficient quantity to substantiate the suspicion of poisoning as an immediate cause of death for the dog. No tablets or drug residue were visually evident in the stomach content.
Antihistamines are H1-receptor antagonists that provide symptomatic relief from allergies and may also be used as sedatives (first-generation). First-generation antihistamines may cause adverse effects because of their cholinergic activity and ability to cross the blood-brain barrier (10). Diphenhydramine is a first-generation ethanolamine-derivative antihistamine widely used in human and veterinary medicine. It is the primary active ingredient in several brand-name OTC cold and sleep aid products such as Benadryl, Nytol, and Tylenol PM.
In humans, diphenhydramine is well-absorbed orally, but undergoes first-pass metabolism in the liver with only 40% to 60% of the drug reaching the systemic circulation. The pharmacokinetics of diphenhydramine have not been studied in canines (11); however, these parameters have been evaluated in humans with peak plasma concentrations occurring within 1 to 5 h and elimination half-lives varying from 2.4 to 10 h (10). A recommended therapeutic dose for diphenhydramine in dogs is 2 to 4 mg/kg BW for the treatment of allergies or mild sedation prior to stressful situations. For an 18-kg dog, this would equate to 36 to 72 mg diphenhydramine or 1 to 1.5 tablets. The margin of safety is relatively narrow within this group of antihistamines, with adverse effects occurring at or less than 1 mg/kg above therapeutic doses (12). Therefore, 2 or more tablets may have been sufficient to initiate a cascade of potentially adverse effects for this dog. However, oral doses of 1, 3, or 10 mg/kg BW have been reported to have no effect on heart rate, mean blood pressure, or electorcardiogram in otherwise healthy dogs (13). Conversely, dogs given 10 mg/kg BW of diphenhydramine in a sleep study had significantly increased drowsiness and non-REM (rapid eye movement) sleep (14).
In living animals, hyperactivity, depression, hypersalivation, tachypnea, and tachycardia are the most common signs reported with ethanolamine-based antihistamines, usually occurring within 1 h of exposure (10). With overdose, dogs may also exhibit mydriasis, dry mucous membranes, disorientation, and fever (10). For animals exposed to an overdose of antihistamines, treatment with guaifenesin and supportive fluid therapy generally results in an excellent prognosis for recovery (15).
The lethal dose (LD50) for diphenhydramine in dogs ranges between 24 to 30 mg/kg BW by IV administration, and death has been attributed to neuromotor excitement and convulsions, followed by respiratory failure and myocardial depression (16). The LD50 for oral diphenhydramine in dogs has not been studied; however, the range may be gleaned from extrapolated values in other species. In humans the minimum lethal dose (LDmin) is 10.1 mg/kg BW and the LD50 in rodents ranges between 114 (mice) and 500 (rats) mg/kg BW (17). Based on this information, the LDmin in this case could have been reached with as few as 4 tablets and the LD50 achieved with approximately 40 tablets. However, with pre-existing multi-systemic pathologies, a lower dose of diphenhydramine may have been sufficient to cause death. For comparison, Lagutchik et al (15) reported a male Labrador retriever dog that ingested an estimated dose of 67 mg/kg BW of diphenhydramine with no concomitant drug exposures. On admission, the serum diphenhydramine concentration was reported at 537 ng/mL and although the concentration associated with toxicity in dogs is unknown, in humans it is > 60 ng/mL (15). With treatment this dog recovered and was discharged 24 h after admission (15).
The additional finding of fatty acid ethyl esters (FAEEs) provides speculative insight into the delivery of the OTC pills, and may be significant to discerning between unintentional and intentional poisoning. These esters are produced by the reaction of fatty acids with ethanol in the presence of the enzyme fatty acid ethyl ester synthase (18), which is present in almost all tissues including the gastric mucosa (19,20). In the described case, the presence of FAEEs indirectly serves as a marker for alcohol consumption. Since the stomach was markedly distended with partially digested food, it stands to reason that alcohol may have been added to the feed and medication mixture to enhance palatability and, hence, ingestion of multiple OTC pills.
Alcohol interacts with a variety of medications (21,22). These interactions may be either pharmacokinetic (affecting metabolism) or pharmacodynamic (enhancing effects) (22). When combined with other medications capable of producing sedation (e.g., antihistamines), alcohol may enhance the sedative effect of those medicines (21). Hence, it could be speculated further that the consumption of alcohol with an overdose of diphenhydramine may have produced an additive, if not lethal, combination.
Interpretation of toxicology results should be in the context of the forensic, crime scene, pathologic, and ancillary diagnostic studies. Simple exposure to a toxicant does not necessarily indicate that a toxicosis has occurred. With all toxic agents, a threshold generally exists below which acute signs will not develop. Technical advancements and the improving ability to measure the presence of toxins at minute levels means we will at times detect agents at levels consistent with casual sublethal exposure but not toxicosis (1). In the current case, the stomach contents were semi-quantitatively estimated to contain 250 ppm diphenhydramine. Based on the size of the dog and degree of gastric distention at the time of necropsy, the stomach volume was estimated to be 500 mL and the amount of diphenhydramine approximated at 125 mg present at the time of sampling. This would have been consistent with an overdose, and did not take into account the quantity of diphenhydramine already absorbed, circulated, and distributed to other body compartments prior to the dogs death and discovery. For comparison, fatal cases in humans have recorded concentrations of 8.7, 12.3, 15, 554, and 705 mg diphenhydramine in the stomach content (23,24). Aside from differences established in gender, age, and weight, variations in the stomach concentration likely reflect the quantity consumed and the temporal relationship between consumption and presentation of the decedent to the medical examiner.
In the case presented, gross pathology did not provide any indication of foul play, rather necropsy and histopathology revealed degenerative conditions that may have left this dog more susceptible to the adverse effects of a drug overdose. In the absence of forensic investigations to evaluate the criminal environment and surrounding motives, malicious poisonings resulting from drug overdose in animals are difficult to prove beyond a reasonable doubt. In summary, thorough pathologic analysis and concomitant analytical toxicology provide invaluable support to a criminal investigation. The analytical evidence described herein suggests the intentional poisoning of this animal with diphenhydramine presented to it in a mixture of feed, drug, and presumably alcohol.
We thank Constable D.M. Reddy from the Integrated Homicide Investigation Team of the Royal Canadian Mounted Police for his review and valuable information regarding the case history. CVJ
Use of this article is limited to a single copy for personal study. Anyone interested in obtaining reprints should contact the CVMA office (gro.vmca-amvc@nothguorbh) for additional copies or permission to use this material elsewhere.