What is the best cream for hives
15 Ways to Get Rid of Hives
You may be able to relieve hives with home remedies, including aloe vera or an oatmeal bath, and over-the-counter products. But a doctor may need to treat severe or chronic hives.
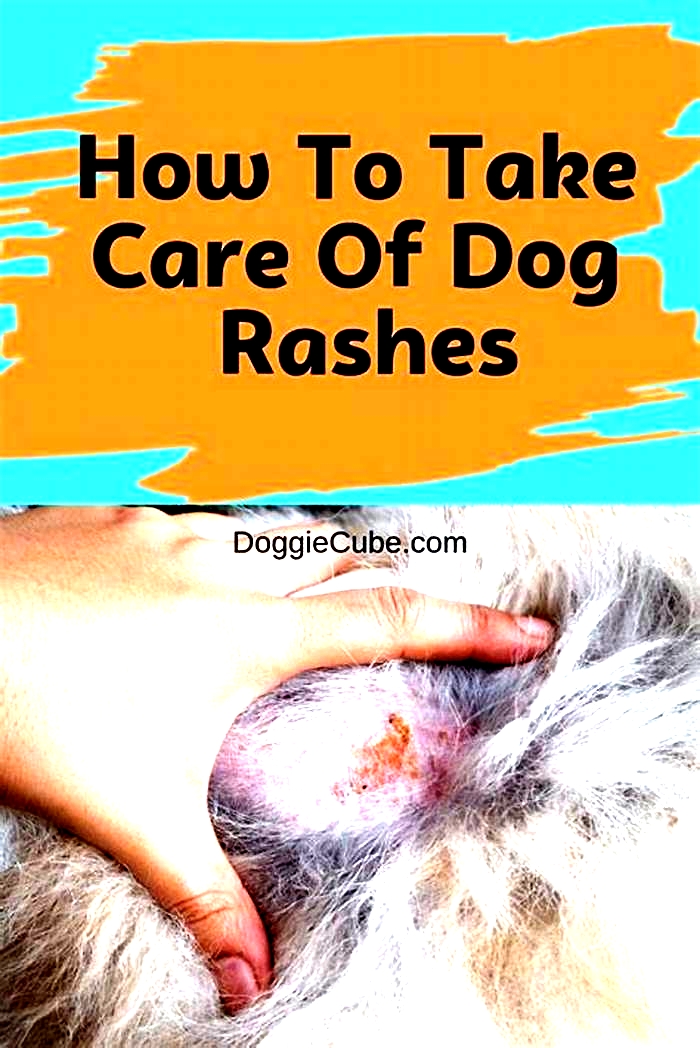
Hives (urticaria) are a rash on your body. Identifying what triggered your hives is crucial to preventing them from happening again. If you can identify the trigger, you can avoid contact with it.
Although hives are often associated with allergic reactions, they can also occur due to:
Hives generally fade within 24 hours and dont require treatment.
However, you should seek immediate medical attention if you experience any of the following:
- dizziness
- swelling in your throat or face
- difficulty breathing
These may indicate a severe allergic reaction and require emergency care.
If your hives are milder, continue reading to learn how to ease any discomfort and speed up the healing process.
Some remedies and other products may cause a skin reaction. Its best to do a skin patch test before applying.
In most cases, home remedies can help you find relief. Here are a few ways to soothe itchy skin:
Use a cold compress
Applying something cool to your skin can help relieve irritation and swelling. To do this, grab a bag of frozen veggies or wrap a handful of ice in a towel and apply it to the affected area for up to 10 minutes. Repeat as needed throughout the day.
Take a bath with an anti-itch solution
There are several products you can add to a bath to relieve itching. These include colloidal oatmeal or one or two handfuls of baking soda.
Learn more: How to make an oatmeal bath
Avoid products that may irritate the skin
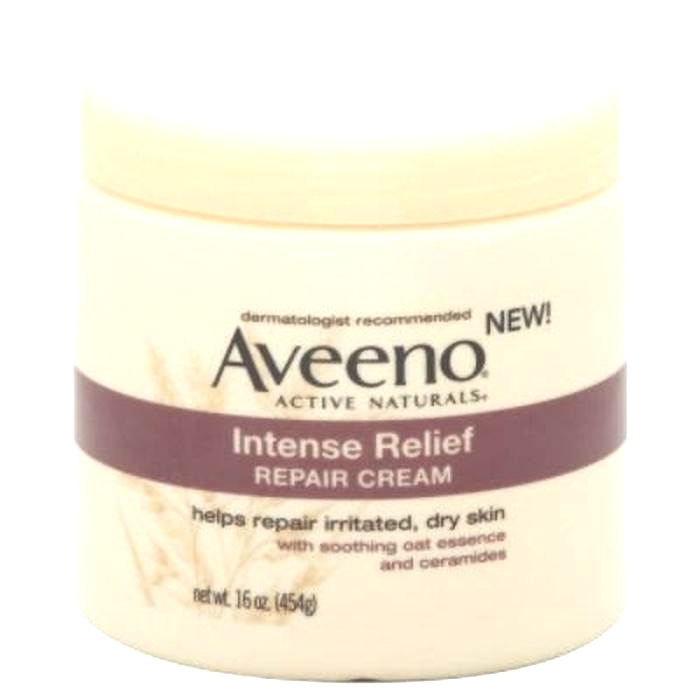
Certain soaps may dry your skin and cause more itching when you have hives. Make sure to use a mild soap thats marketed for sensitive skin. These typically omit fragrance and irritating chemicals.
You should also avoid using irritating moisturizers or lotions. When in doubt, opt for a formula that targets sensitive skin, such as these options. Applying immediately after bathing may also help soothe the itch.
Keep things cool
Heat can make itchiness worse. Wear lightweight clothing and keep the temperature in your house cool and comfortable. Avoid sitting in direct sunlight.
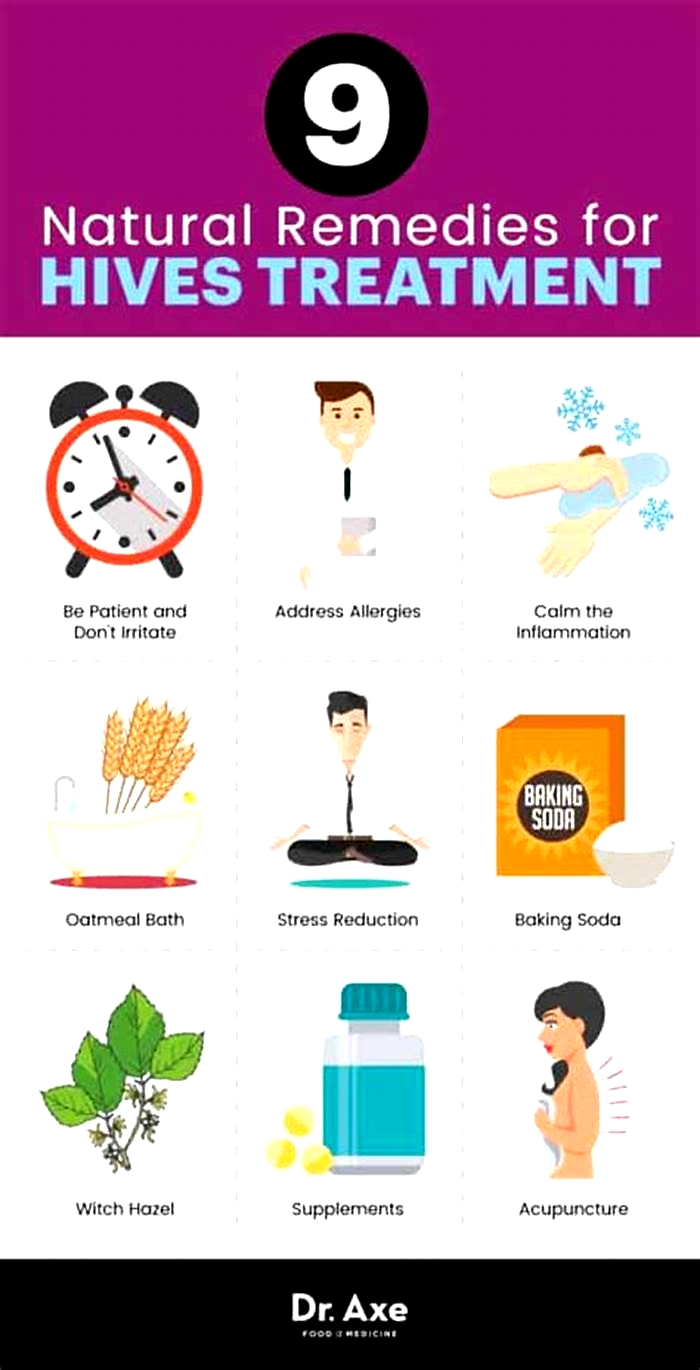
If home remedies arent relieving your symptoms but you arent ready to head to the pharmacy you may want to give a few natural solutions a try.
Natural remedies arent regulated or approved by the Food and Drug Administration (FDA), so use them with caution.
Witch hazel
The natural tannins found in the herb witch hazel can help relieve irritation. Despite this, it
You can apply witch hazel to your skin like a mask a few times each day. Let it sit on the affected areas for about 20 minutes, and then rinse it off.
Aloe vera
Aloe vera is a natural anti-inflammatory. According to the
But, as with any new product, its important to do a skin patch test before application, especially if you have sensitive skin. Some aloe products may also have added fragrance or other chemicals, so be sure to read the label.
You can apply topical aloe vera to your hives as needed, likely a few times a day. Be sure to follow any instructions on the package.
If the above remedies arent enough to help your hives, over-the-counter (OTC) treatments may help relieve your symptoms. Not only can OTC options relieve itching and irritation, but they can also target your bodys histamine response, which is what causes hives.
Calamine lotion
Products containing calamine can help relieve itching by cooling your skin. You can apply calamine lotion directly to your skin:
- Make sure you mix the lotion before using it by shaking the container.
- Put some calamine lotion on a cotton pad or cloth.
- Apply the pad or cloth directly to the hives and let dry.
You can treat the hives with calamine lotion as necessary.
Diphenhydramine (Benadryl)
This oral antihistamine can reduce rash and other allergy symptoms like itching by working from the inside out.
Be sure to follow the dosage instructions on the package. Benadryl usually kicks in within an hour and should start to relieve your symptoms the same day.
Benadryl may cause drowsiness.
Fexofenadine (Allegra), loratadine (Claritin), and cetirizine (Zyrtec)
These antihistamines typically come in 12- or 24-hour formulas to provide extended relief. Theyre also less likely to cause drowsiness than diphenhydramine.
You may need to adjust the dosage to effectively treat hives, so talk with a doctor or pharmacist. They can advise you on how much to take and how often.
If youre experiencing severe or chronic hives, you may need prescription medication. Talk with a doctor about your symptoms and how you can best find relief.
Common prescription options include:
Prednisone (Deltasone)
This corticosteroid is taken orally. You should only use it for a short period of time as directed by a doctor. Corticosteroids can have side effects, especially if taken for extended periods of time. Side effects can include:
- elevated blood pressure
- elevated eye pressure (glaucoma)
- swelling
- weight gain
- immunosuppression, which means you may get infections more easily
To reduce side effects, take oral corticosteroids at a lower dose and transition to corticosteroid creams with your doctors supervision.
Omalizumab (Xolair)
This medication must be injected under the skin. This option is
- headache
- dizziness
- inner ear pain
- cold symptoms
Dapsone (Aczone)
This antibiotic is available topically and as an oral medication. This medication can treat inflammation due to hives or other skin conditions that are caused by bacterial infection. Its important to take all antibiotics as prescribed.
Antibiotics only help relieve symptoms caused by a bacterial infection.
Leukotriene-receptor antagonists
This nonsteroidal treatment option is taken orally. These drugs should be used only after steroid treatment and antihistamines have been unsuccessful. There is
- headache
- nausea
- cough
- low fever
If your symptoms worsen or last longer than a couple of days, you may want to talk with a doctor. They can identify the cause and provide medication to help relieve your symptoms. Understanding your triggers may help prevent future outbreaks.
10 ways to get relief from chronic hives
 Biosimilars: 14 FAQs
Biosimilars: 14 FAQsFind answers to questions patients ask about this newer treatment option, including, Whats involved in switching from a biologic to a biosimilar?
Featured
 Laser hair removal
Laser hair removalYou can expect permanent results in all but one area. Do you know which one?
 Scar treatment
Scar treatmentIf you want to diminish a noticeable scar, know these 10 things before having laser treatment.
 Botox
BotoxIt can smooth out deep wrinkles and lines, but the results arent permanent. Heres how long botox tends to last.
Featured
 Find a Dermatologist
Find a DermatologistYou can search by location, condition, and procedure to find the dermatologist thats right for you.
 What is a dermatologist?
What is a dermatologist?A dermatologist is a medical doctor who specializes in treating the skin, hair, and nails. Dermatologists care for people of all ages.
Chronic hives
Diagnosis
To diagnose chronic hives, your health care provider will likely talk with you about your symptoms and look at your skin. One of the telling features of chronic hives is that the welts come and go at random. You might be asked to keep a diary to keep track of:
- Your activities
- Any medications, herbal remedies or supplements you take
- What you eat and drink
- Where hives appear and how long it takes a welt to fade and whether it leaves behind a bruise or other mark
- Whether your hives come with painful swelling
You may also need blood tests to determine the cause of your symptoms. An accurate diagnosis will guide your treatment options. If needed to clarify the diagnosis, your doctor might take a skin sample (biopsy) to examine under a microscope.
Treatment
Treatment for chronic hives often starts with nonprescription anti-itch drugs (antihistamines). If these don't help, your health care provider might suggest that you try one or more of these treatments:
Prescription anti-itch drugs. The usual treatment for chronic hives is prescription antihistamine pills that don't make you drowsy. These drugs ease itching, swelling and other allergy symptoms. Daily use of these drugs helps block the symptom-producing release of histamine. Examples include:
- Cetirizine
- Desloratadine (Clarinex)
- Fexofenadine
These medications have few side effects. If the nondrowsy antihistamines don't help you, your health care provider may increase the dose or add another type of antihistamine.
Check with your health care provider before taking any of these medications if you're pregnant or breastfeeding, have a long-term medical condition, or take other medications.
Other medications
If the first-choice drugs don't ease your symptoms, other drugs may help. For example:
- Famotidine (Pepcid AC)
- Montelukast (Singulair)
- Doxepin (Silenor, Zonalon)
- Cimetidine (Tagamet HB)
- Nizatidine (Axid AR)
- Ranitidine (Zantac)
- Omalizumab (Xolair)
For chronic hives that resist these treatments, your health care provider might prescribe a drug that can calm an overactive immune system. Examples are cyclosporine (Gengraf, Neoral, Sandimmune), tacrolimus (Prograf, Protopic, others), hydroxychloroquine (Plaquenil) and mycophenolate (Cellcept, Myfortic).
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Chronic hives can go on for months and years. They can interfere with sleep, work and other activities. The following self-care tips may help you manage your condition:
- Avoid triggers. These can include foods, medications, pollen, pet dander, latex and insect stings. If you think a medication caused your welts, stop using it and contact your primary care provider. Some studies suggest that stress or fatigue can trigger hives.
- Use a nonprescription anti-itch drug. A nonprescription anti-itch (antihistamine) pill that doesn't cause drowsiness may help ease itching. Examples include loratadine (Alavert, Claritin, others) and cetirizine (Zyrtec Allergy).
- Apply cold. Soothe the skin by covering the itchy area with a cold washcloth or rubbing an ice cube over it for a few minutes.
- Take a comfortably cool shower or bath. Some people might relieve itching in the short term by taking a cool shower or bath. Try sprinkling the bath water with baking soda or oatmeal powder (Aveeno, others).
- Apply an anti-itch cream or lotion. Try a cream with menthol for a soothing effect.
- Wear loose, smooth-textured cotton clothing. Avoid wearing clothing that's rough, tight, scratchy or made from wool.
- Protect your skin from the sun. Liberally apply sunscreen about a half hour before going outdoors. When outdoors, seek shade to help relieve discomfort.
- Track your symptoms. Keep a diary of when and where hives occur, what you were doing, what you were eating, and so on. This may help you and your health care provider identify triggers.
Preparing for your appointment
You'll likely start by seeing your primary care provider. Or you may be referred to an allergy specialist or a doctor who specializes in the diagnosis and treatment of skin conditions (dermatologist).
What you can do
Here are some tips to help you get ready for your appointment.
- List your symptoms, when they occurred and how long they lasted.
- List any medications you're taking, including vitamins, herbs and supplements. Even better, take the original bottles and a list of the doses and directions.
- List questions to ask your doctor.
For chronic hives, questions you may want to ask include:
- What is likely causing my symptoms?
- How long will hives last?
- What kinds of tests do I need? Do these tests require any special preparation?
- What treatments are available, and which do you suggest?
- What are the alternatives to the primary approach that you're suggesting?
- Do these treatments have any side effects?
- Do I need prescription medication, or can I use nonprescription drugs to treat the condition?
- Does the medicine you're prescribing have a generic version?
What to expect from your doctor
Your health care provider is likely to ask you a few questions, such as:
- When did you first have symptoms?
- What did your skin reaction look like when it first appeared?
- Have your symptoms changed over time?
- Have you noticed anything that makes your symptoms worse or better?
- Do your skin lesions mainly itch, or do they burn or sting?
- Do your skin lesions go away completely without leaving a bruise or a mark?
- Do you have any known allergies?
- Have you ever had a similar skin reaction before?
- Have you tried a new food for the first time, changed laundry products or adopted a new pet?
- What prescriptions, nonprescription medications and supplements are you taking?
- Have you started taking any new medications or started a new course of a medication you've taken before?
- Has your overall health changed recently? Have you had any fevers or have you lost weight?
- Has anyone else in your family ever had this kind of skin reaction? Do other family members have any known allergies?
- What at-home treatments have you used?