What is the strongest antihistamine for hives

Chronic hives
Diagnosis
To diagnose chronic hives, your health care provider will likely talk with you about your symptoms and look at your skin. One of the telling features of chronic hives is that the welts come and go at random. You might be asked to keep a diary to keep track of:
- Your activities
- Any medications, herbal remedies or supplements you take
- What you eat and drink
- Where hives appear and how long it takes a welt to fade and whether it leaves behind a bruise or other mark
- Whether your hives come with painful swelling
You may also need blood tests to determine the cause of your symptoms. An accurate diagnosis will guide your treatment options. If needed to clarify the diagnosis, your doctor might take a skin sample (biopsy) to examine under a microscope.
Treatment
Treatment for chronic hives often starts with nonprescription anti-itch drugs (antihistamines). If these don't help, your health care provider might suggest that you try one or more of these treatments:
Prescription anti-itch drugs. The usual treatment for chronic hives is prescription antihistamine pills that don't make you drowsy. These drugs ease itching, swelling and other allergy symptoms. Daily use of these drugs helps block the symptom-producing release of histamine. Examples include:
- Cetirizine
- Desloratadine (Clarinex)
- Fexofenadine
These medications have few side effects. If the nondrowsy antihistamines don't help you, your health care provider may increase the dose or add another type of antihistamine.
Check with your health care provider before taking any of these medications if you're pregnant or breastfeeding, have a long-term medical condition, or take other medications.
Other medications
If the first-choice drugs don't ease your symptoms, other drugs may help. For example:
- Famotidine (Pepcid AC)
- Montelukast (Singulair)
- Doxepin (Silenor, Zonalon)
- Cimetidine (Tagamet HB)
- Nizatidine (Axid AR)
- Ranitidine (Zantac)
- Omalizumab (Xolair)
For chronic hives that resist these treatments, your health care provider might prescribe a drug that can calm an overactive immune system. Examples are cyclosporine (Gengraf, Neoral, Sandimmune), tacrolimus (Prograf, Protopic, others), hydroxychloroquine (Plaquenil) and mycophenolate (Cellcept, Myfortic).
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Chronic hives can go on for months and years. They can interfere with sleep, work and other activities. The following self-care tips may help you manage your condition:
- Avoid triggers. These can include foods, medications, pollen, pet dander, latex and insect stings. If you think a medication caused your welts, stop using it and contact your primary care provider. Some studies suggest that stress or fatigue can trigger hives.
- Use a nonprescription anti-itch drug. A nonprescription anti-itch (antihistamine) pill that doesn't cause drowsiness may help ease itching. Examples include loratadine (Alavert, Claritin, others) and cetirizine (Zyrtec Allergy).
- Apply cold. Soothe the skin by covering the itchy area with a cold washcloth or rubbing an ice cube over it for a few minutes.
- Take a comfortably cool shower or bath. Some people might relieve itching in the short term by taking a cool shower or bath. Try sprinkling the bath water with baking soda or oatmeal powder (Aveeno, others).
- Apply an anti-itch cream or lotion. Try a cream with menthol for a soothing effect.
- Wear loose, smooth-textured cotton clothing. Avoid wearing clothing that's rough, tight, scratchy or made from wool.
- Protect your skin from the sun. Liberally apply sunscreen about a half hour before going outdoors. When outdoors, seek shade to help relieve discomfort.
- Track your symptoms. Keep a diary of when and where hives occur, what you were doing, what you were eating, and so on. This may help you and your health care provider identify triggers.
Preparing for your appointment
You'll likely start by seeing your primary care provider. Or you may be referred to an allergy specialist or a doctor who specializes in the diagnosis and treatment of skin conditions (dermatologist).
What you can do
Here are some tips to help you get ready for your appointment.
- List your symptoms, when they occurred and how long they lasted.
- List any medications you're taking, including vitamins, herbs and supplements. Even better, take the original bottles and a list of the doses and directions.
- List questions to ask your doctor.
For chronic hives, questions you may want to ask include:
- What is likely causing my symptoms?
- How long will hives last?
- What kinds of tests do I need? Do these tests require any special preparation?
- What treatments are available, and which do you suggest?
- What are the alternatives to the primary approach that you're suggesting?
- Do these treatments have any side effects?
- Do I need prescription medication, or can I use nonprescription drugs to treat the condition?
- Does the medicine you're prescribing have a generic version?
What to expect from your doctor
Your health care provider is likely to ask you a few questions, such as:
- When did you first have symptoms?
- What did your skin reaction look like when it first appeared?
- Have your symptoms changed over time?
- Have you noticed anything that makes your symptoms worse or better?
- Do your skin lesions mainly itch, or do they burn or sting?
- Do your skin lesions go away completely without leaving a bruise or a mark?
- Do you have any known allergies?
- Have you ever had a similar skin reaction before?
- Have you tried a new food for the first time, changed laundry products or adopted a new pet?
- What prescriptions, nonprescription medications and supplements are you taking?
- Have you started taking any new medications or started a new course of a medication you've taken before?
- Has your overall health changed recently? Have you had any fevers or have you lost weight?
- Has anyone else in your family ever had this kind of skin reaction? Do other family members have any known allergies?
- What at-home treatments have you used?
How to Treat Hives
If you have only one outbreak of hives and you dont have breathing difficulties, you probably dont need medical attention. Yet if you continue to get multiple bouts of hives that continue after a couple of weeks, you may want to call a doctor, Elmariah suggests. Most often, the hives will resolve during this time or youll figure out whats causing them.
But hives that continue for weeks warrant a trip to a specialist, such as a dermatologist or an allergist. If they continue for six weeks or longer theyre considered chronic hives, which tend to be caused by the same triggers as short-term or acute cases of hives. Because dermatologists and allergists are skilled at working with hives, theyre your best bet for getting appropriate treatment, Dr. Rossi explains.
How Doctors Diagnose Hives
Expect to undergo a thorough physical exam. The dermatologist or allergist will also likely ask you to review your hives experience in detail, including when the hives started, if you suspect anything in particular triggered your hives, what medications youve tried, and what type of response youve gotten. Come prepared with this information.
Doctors will also verify that the bump (or bumps) is hives, often circling the spot on your skin to see if it disappears the next day (if so, its a hive, Elmariah says).
Once theyve confirmed that it is hives, theyll work to determine the trigger. Rossi says: Figuring out the cause can be the most frustrating part of it, especially if the tests arent helpful.
You may require additional testing. If an allergy is suspected, you may need to undergo allergy testing. If you are diagnosed with a severe allergy, the doctor may prescribe an epinephrine auto-injector (such as an EpiPen) in case youre accidentally exposed to your allergen. (1)
And because chronic hives can signal autoimmune disorders, you may need to have a blood draw in which doctors will look for a common antibody found in many autoimmune disorders. In rare cases when a bout of hives doesnt disappear within 24 hours, your doctor may do a skin biopsy to see if theres inflammation of the blood vessels, Rossi adds.
Treatments Doctors Use for Hives
Doctors usually prescribe antihistamines as the first course of treatment for hives. Acute cases can generally be treated with over-the-counter antihistamines like loratadine and pseudoephedrine,cetirizine, fexofenadine, or diphenhydramine.
If your hives are persisting (or youve already tried OTC antihistamines without success), your doctor may move to another class of antihistamines called histamine type 2 receptor antagonists, or H2 blockers, including cimetidine (Tagamet) and famotidine (Pepcid)(both available over the counter); up the dose of antihistamines (some as high as four times); or combine several antihistamines, Friedman says.
In some cases, your doctor may prescribe an oral steroid, such asprednisone (Deltasone), if your hives still arent responding. Oral steroids are stronger but can cause more significant side effects than antihistamines. (3)
If youre still not seeing results, your doctor may recommend even stronger medications, like an injectable prescription medication called omalizumab(Xolair). There is also evidence that off-label use of stronger medications that suppress the immune system under careful monitoring by a specialist may be helpful in patients with difficult-to-manage hives.
Its important to note that you shouldnt try taking high doses of vitamins or any other off-label medication on your own without instruction from your doctor. No one treatment works for everyone, Friedman says. And for some, such therapies may not be safe.
Fexofenadine - Brand names: Almerg, Telfast, Treathay
If you or your child have been prescribed fexofenadine, follow your doctor's instructions about how and when to take it.
Dosage
Fexofenadine comes as tablets in different strengths: 30mg, 120mg and 180mg.
How much you take depends on why you're taking it.
The usual dose for treating hay fever is:
- 120mg once a day for adults and children aged 12 years and over
- 30mg twice a day for children aged 6 to 11 years, with the doses spaced 10 to 12 hours apart
The usual dose for treating hives is 180mg once a day for adults and children aged 12 years and over.
Fexofenadine is not recommended for treating hives in children under 12.
How to take it
If you're taking 30mg fexofenadine tablets, you can take them with or without food.
If you're taking 120mg or 180mg fexofenadine tablets, take them before a meal.
Always take your fexofenadine tablets with a drink of water. Swallow them whole do not chew them.
When to take it
Try to take fexofenadine tablets at about the same time every day. Choose a time that is easy to remember.
You may only need to take fexofenadine on a day you have symptoms, such as when you've been exposed to something you're allergic to, like animal hair.
Or you may need to take it regularly to prevent symptoms, such as to stop hay fever during spring and summer.
What if I forget to take it?
If you're taking fexofenadine once a day, take your forgotten dose as soon as you remember, unless it's nearly time for your next dose. In this case, skip the missed dose and take your next dose at the usual time.
Do not take 2 doses to make up for a forgotten dose.
If you forget to give a dose to a child who is taking fexofenadine twice a day, you can give the dose if it's within 4 hours of when they should have had it.
If you remember more than 4 hours after, do not give the missed dose. Instead, wait until the next dose and carry on as normal.
If you often forget doses, it may help to set an alarm to remind you. You could also ask your pharmacist for advice on other ways to help you remember to take your medicine.
What if I take too much?
Fexofenadine is generally very safe. Taking more than your usual dose is unlikely to harm you.
If you take an extra dose, you might get some of the common side effects. If this happens or you're concerned, contact your doctor.
What to Do When Antihistamines Arent Working for Hives
Antihistamines may not work for some people, depending on the severity of their hives. You may need an increased dosage or a different medication altogether.
After a chronic idiopathic urticaria (CIU) diagnosis, your doctor will likely prescribe an oral antihistamine to treat your symptoms. However, antihistamines arent always effective.
If youve already tried an antihistamine and you arent seeing results, schedule an appointment with your doctor to learn about possible next steps.
Here are some questions you can ask your doctor at your follow-up appointment and some information about what you might hear in response.
Its hard to say why antihistamines work for some people and not for others. But its not uncommon for antihistamines to be or become ineffective.
Research on the effectiveness of antihistamines for chronic hives has shown a response rate as low as
Antihistamines may stop working because hives can become worse over time or because the intensity of hives can wax and wane over time.
Its also possible that antihistamines become less effective because people arent taking them as prescribed.
Even if you cant identify the cause of your CIU, you may be able to pinpoint triggers that bring on outbreaks or increase the severity of your hives.
See whether any of the following common triggers seem to affect you:
- pets or pet dander
- exposure to extreme heat or cold
- exposure to direct sunlight
- vigorous exercise
- pressure on the skin
- stress or anxiety
- nonsteroidal anti-inflammatory drugs (like ibuprofen)
By understanding your personal triggers, you can put yourself in a better position to avoid them.
After seeing little to no results from an antihistamine, your doctor may suggest that you try the following treatments, usually in the following order:
- Higher dose: Sometimes increasing the dose of your current antihistamine can yield better results.
- A different antihistamine or a combination of several different antihistamines. Your doctor may consider switching you to a different antihistamine or putting you on a regimen of two types of antihistamines. For example, they may recommend an H1-antihistamine combined with an H2-antihistamine, which targets different receptors in the body.
- Oral corticosteroids. While doctors usually dont recommend prolonged use of steroids due to potential side effects, they may recommend a short course. This is especially likely if your hives are severe or if theyre accompanied by swelling.
- Cyclosporine (Gengraf, Neoral, Sandimmune): This is an immunosuppressant drug that has led to remission from hives in
50% of cases , according to research. - Omalizumab (Xolair). Your doctor may recommend omalizumab, a medication thats injected once a month if your hives are difficult to treat, but is effective in 80% of cases.
- Leukotriene receptor antagonists (LTRAs): Two drugs, zafirlukast (Accolate) and montelukast, might be prescribed in cases of hives caused by Aspirin, and there isnt enough data on their effectiveness on hives overall.
If your medication isnt giving you the relief you need, you can try the following methods to ease itching:
- Moisturize regularly with lotion.
- Use cool water when you shower.
- Apply a cold compress or an ice pack to affected areas.
- Try using over-the-counter creams such as calamine lotion.
- Wear loose clothing made from 100% cotton or 100% silk.
While none of the above methods will treat your CIU, they can at least provide comfort during a flare-up.
Dietary changes to help prevent hives
Researchers are still studying whether changing your diet can impact the severity and duration of CIU flare-ups.
A 2018 preliminary Korean study suggests that an antihistamine diet, where you avoid foods that contain high levels of histamine, may help reduce the severity on an individual level.
Since this and other similar studies only involved a small group of participants, researchers arent ready to draw wide conclusions about the diets success rate.
Even so, it may be worth talking with your doctor to see whether changing your diet is a good option.
No. Hives are never contagious, so you dont need to worry about spreading them to friends, family members, or others who are in close contact.
You also dont have to worry about the hives spreading if you touch other parts of your body after touching your hives.
If youre concerned about what other people will think when they see the welts on your skin, you can ask your doctor to provide a note explaining the nature of CIU and its symptoms. This can be especially useful for school-aged children.
No. While it may be frustrating to learn that antihistamines arent effective at treating your hives, you dont need to worry that they will leave any permanent marks or scars.
Most hives last for no longer than 24 hours and should fade and disappear after that.
While most cases of CIU arent dangerous, there are several warning signs that you should be aware of. Sudden and severe hives can mean youre experiencing an allergic reaction and need urgent medical attention.
If you experience any of the symptoms of anaphylaxis alongside a hives outbreak, call 911 or go to the emergency room:
By definition, chronic means that your hives will last for 6 weeks or more. But theres no way to say for sure exactly how long a specific outbreak episode will last. It could be months or even years.
Each individual welt will probably last for several hours, but theyre often quickly replaced by new ones.
The good news is that CIU can go away, its just hard to predict when.
Should I see an allergist?
If youve already been diagnosed with CIU, your doctor believes the cause is unknown and an allergy isnt to blame. But if you suspect that your doctor overlooked an underlying allergy, you may want to consider seeing an allergist.
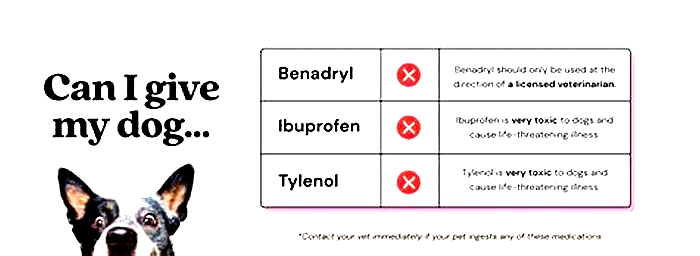
What happens if hives dont go away with Benadryl?
Benadryl (diphenhydramine) is an over-the-counter antihistamine that can be used to treat mild allergic reactions, including hives. It is an H1 antihistamine, which means it is one of the ones your doctor may want you to try first. It is also available in higher doses as a prescription if the OTC version doesnt work for you. If its still ineffective, your doctor will likely switch you to H2 antihistamines, other medications, or a combination of drugs.
Why is Benadryl not stopping my allergic reaction?
If there is an ongoing trigger for your hives in your environment, you might continue to develop them or they may worsen even if youre taking an antihistamine like Benadryl. In addition to taking medication, its important to try to identify the trigger and eliminate it. To do this, make an appointment with a dermatologist or allergist for testing, and track your flare-ups. That said, sometimes there is no identifiable cause. Make sure you are taking your medication exactly as prescribed or following the directions on the box of any OTC drug.
If antihistamines dont work for you, dont become discouraged. This happens for certain people and under certain circumstances.
Ask your doctor about possible next steps. Whether that involves a different form of medication or introducing some natural steps to reduce itching, you have options to decrease CIU-related discomfort.