When to worry about hives

Hives and angioedema
Overview
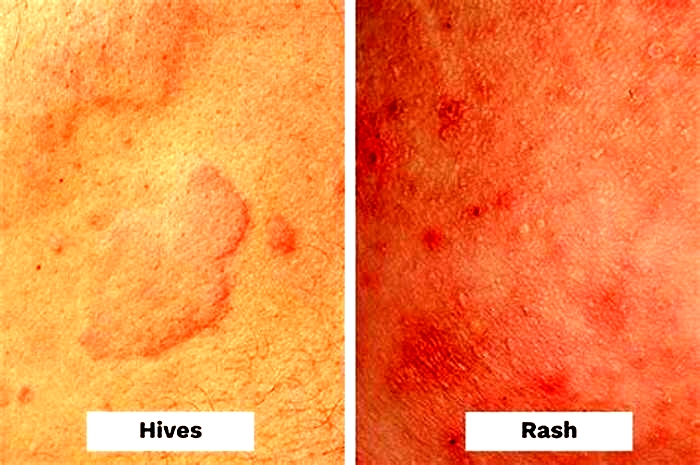
Hives
Hives
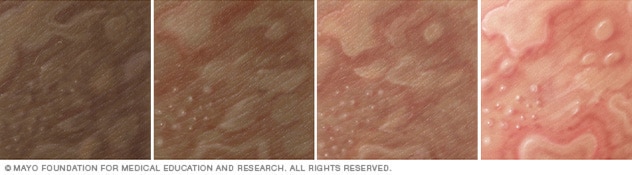
Illustration of hives on different skin colors. Hives can cause swollen, itchy welts. Hives is also called urticaria.
Angioedema
Angioedema
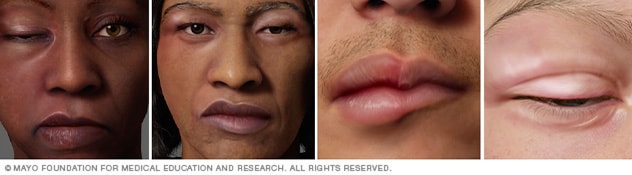
Illustration of angioedema on different skin colors. Angioedema causes swelling in the deeper layers of skin, often of the face and lips. It often goes away within a day.
Hives also known as urticaria (ur-tih-KAR-e-uh) is a skin reaction that causes itchy welts that range in size from small spots to large blotches. Hives can be triggered by many situations and substances, including certain foods and medications.
Angioedema can arise with hives or alone. It causes swelling in the deeper layers of skin, often around the face and lips. Short-lived (acute) hives and angioedema are common. Most times, they are harmless, clear up within in a day and don't leave any lasting marks, even without treatment. Hives that last longer than six weeks are called chronic hives.
Hives and angioedema are usually treated with antihistamine medication. Angioedema can be life-threatening if swelling of the tongue or in the throat blocks the airway.
Symptoms
Hives
The welts associated with hives can be:
- Skin-colored, reddish on white skin, or purplish on black and brown skin
- Itchy, ranging from mild to intense
- Round, oval or worm-shaped
- As small as a pea or as large as a dinner plate
Most hives appear quickly and go away within 24 hours. This is known as acute hives. Chronic hives can last for months or years.
Angioedema
Angioedema is a reaction similar to hives that affects deeper layers of the skin. It can appear with hives or alone. Signs and symptoms include:
- Welts that form in minutes to hours
- Swelling, especially around the eyes, cheeks or lips
- Mild pain and warmth in the affected areas
When to see a doctor
You can usually treat mild cases of hives or angioedema at home. See your health care provider if your symptoms continue for more than a few days.
If you think your hives or angioedema was caused by a known allergy to food or a medication, your symptoms may be an early sign of an anaphylactic reaction. Seek emergency care if you feel your tongue, lips, mouth or throat swelling or if you're having trouble breathing.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
ErrorEmail field is required
ErrorInclude a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Causes
For most people who experience acute hives and angioedema, the exact cause can't be identified. The conditions are sometimes caused by:
- Foods. Many foods can trigger reactions in people with sensitivities. Shellfish, fish, peanuts, tree nuts, soy, eggs and milk are frequent offenders.
- Medications. Many medications may cause hives or angioedema, including penicillins, aspirin, ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve) and blood pressure medications.
- Airborne allergens. Pollen and other allergens that you breathe in can trigger hives, sometimes accompanied by upper and lower respiratory tract symptoms.
- Insect bites and infections. Other causes of acute hives and angioedema are insect bites and infections.
Risk factors
Hives and angioedema are common. You may be at increased risk of hives and angioedema if you:
- Have had hives or angioedema before
- Have had other allergic reactions
- Have a family history of hives, angioedema or hereditary angioedema
Complications
Severe angioedema can be life-threatening if swelling of the tongue or in the throat blocks the airway.
Prevention
To lower your likelihood of experiencing hives or angioedema, take the following precautions:
- Avoid known triggers. If you know what has triggered your hives, try to avoid that substance.
- Bathe and change your clothes. If pollen or animal contact has triggered your hives in the past, take a bath or shower and change your clothes if you're exposed to pollen or animals.
Oct. 27, 2023
Hives (Urticaria)
What are hives?
Hives, or urticaria, are flat red welts that can appear anywhere on the skin and usually itch. Hives often occur as an allergic reaction to something eaten or something that has contacted the skin. Foods, medicines, and plants are common causes, but sun exposure, stress, infections, and autoimmune diseases have also been known to cause hives.
Symptoms include an itchy, stinging pink rash of slightly swollen skin. The rash may wax and wane in severity. Acute hives typically resolve within six weeks, but chronic hives (urticaria) can persist for months or years.
Hives often resolve on their own, especially in children. Otherwise, treatment for acute hives involves oral antihistamine medications to help relieve the itching and stinging. Chronic hives that do not improve with antihistamines may be treated additionally with corticosteroids, antibiotics, and other stronger medicines. A study found that 35% of people with chronic hives, are symptom free within one year, with another 29% having some reduction of symptoms.
You can safely treat this condition on your own as long as you does not develop trouble breathing. Any antihistamine (like Zyrtec, Clarinex, etc) works.
Viral Hives In Children: What Doctors Want You To Know
You put your sleepy, slightly stuffed-up toddler down for a nap, and when you go to pick them up an hour or two later, you notice splotchy, slightly raised, red spots on their skin. Did you know that the stuffy nose whether its from an RSV infection, or some other, common cold virus could be the culprit? Viral hives in children are incredibly common, and in fact, viral infections are the most common reason that children experience hives, Dr. Natasha Burgert, a board-certified pediatrician, tells Romper. But what viruses cause hives, or urticaria (the clinical name for hives), in children? And how can you be sure that the red, slightly itchy rash on your childs body is viral hives and not something more concerning? While its always a good idea to check in with your pediatrician when you notice something new, once youve confirmed a diagnosis of viral hives, you should be able to breathe a little easier, as they are generally not difficult to manage at home.
What are viral hives?
Before we get into the specifics of viral hives, perhaps we should define hives themselves, which can be caused by a virus or an allergic reaction. Hives are a local inflammatory reaction caused by release multiple mediators resulting in red, raised lesions that are very itchy, says Dr. Mark Toney, Division Chief of Hospital Pediatrics, Nemours Children's Health at Wolfson Childrens Hospital. Viral hives, as the name suggests, are simply hives that are caused by a virus. Viral hives are:
Rashes with viral infections are common in children, explains Dr. Maureen Bauer, a specialist in Pediatric Allergy & Immunology at Children's Hospital Colorado. So, viral hives are when the rash looks like hives-red, raised and itchy.
How long do viral hives last in children?
While viral hives are often short-lived, it is not unusual for them to last anywhere from a few days to weeks. There is a range but typically they last days to a few weeks, says Bauer. Our experts agree that nailing down the exact timeline can be tricky, as young children can get multiple viruses in succession. Individual hives can appear and worsen over minutes to hours and then typically disappears in 24 hours. This cycle can occur over 1-3 weeks usually, Toney explains, adding that chronic hives is defined as this pattern lasting longer than 6 weeks.
However, Burgert is quick to add that true chronic hives are very rare, and particularly hard to diagnose: Idiopathic or recurring hives can be tricky to diagnose since young children commonly get back-to-back viral illness. With each infection, it's possible for a new round of hives to develop. This repeated cycle can make it appear like the hives are chronic, rather than simply a symptom of frequent infections.
What viral infections cause hives in children?
Viral hives in children are so common that, typically, your pediatrician will not test to find out which virus is causing them. Our experts agree that the list of viruses that can cause hives is long, and includes:
But, specific viruses aside, exactly what is going on in your childs immune system that causes them to break out in hives? The infection-fighting power of a child's immune system causes viral hives, Burgert explains. As the immune system ramps up, various body cells are called into action, including those that release histamine. When histamine is released into the bloodstream, hives may develop on the skin.
How do you treat viral hives in children?
Knowing that viral hives in children much like their allergy-induced counterparts are caused by a histamine reaction, you may suspect that an antihistamine is the way to go in terms of treating viral hives at home. Once youve confirmed checked in with your pediatrician, our experts agree that home care is sufficient for viral hives in children.
If the viral hives are not bothering your child, you can opt not to treat them at all.
Beyond that, treatment is something parents should talk to their doctor about, encourages Bauer. Typically, we would recommend using a non-sedating antihistamine to help until they go away. The hives typically resolve when the viral infection is gone. If your child is itchy or seems to be bothered by the hives, Burget suggests the following:
- Long-acting antihistamines, like Zyrtec or Claritin, for children as young as 6 months
- Topical over-the-counter hydrocortisone to lessen itch
- Topical calamine lotion to lessen itch and discomfort
- Oatmeal baths and ice packs to relieve and soothe itching skin
Hives that occur during or after viral illnesses are not harmful to children, but can be annoyingly uncomfortable, explains Burgert. The good news is that this type of rash can be easily managed.
Hives in toddlers that go come and go: Why does this happen?
You noticed a little rash on your childs skin, but it disappeared right when you were about to call the doctor about it, only to maddeningly reappear the next morning. It may strike you as strange to see a skin reaction come and go, but in fact, the come and go is classic for hives and actually helps us in separating this from other, more worrisome rashes, explains Toney. The local reaction can occur throughout the course of the illness and involve various skin locations at different times. There will also be a response when the antihistamine is working and when it starts to wear off.
When to worry about hives in children
Hives become a medical emergency if they are associated with any of the following respiratory symptoms, according to Toney:
- Bad cough
- Wheezing
- Any difficulty in breathing
Parents should connect with their pediatrician for advice if they notice the rash:
- Becomes painful to the touch
- Isnt improving with simple over-the-counter medications
- Looks more like a bruise
- Lasts for more than a few days
Hives due to a food allergy are more concerning, but will typically happen reproducibly in 1-2 hours after eating the food and are often accompanied by other symptoms, says Bauer. If parents notice hives in relation to a particular trigger they should talk to their doctor.
If your child seems to be feeling alright, breathing normally and your pediatrician has confirmed that their rash appears to be viral hives, you should be fine to manage them at home with TLC and maybe an OTC antihistamine. That said, I hold a lot of value in parent perception of the acuity of their child, Toney adds. The above symptoms are definite, but when a parents concern is raised, they should get their child evaluated.
Experts:
Dr. Natasha Burgert, M.D., a board-certified pediatrician
Dr. Mark Toney, M.D., Division Chief of Hospital Pediatrics, Nemours Children's Health at Wolfson Childrens Hospital
Dr. Maureen Bauer, M.D., a specialist in Pediatric Allergy & Immunology at Children's Hospital Colorado
This article was originally published on