Why are hives not going away

Hives That Wont Go Away: The Basics of CIU | Asthma and Allergy Foundation of America
Hives, those annoying itchy red bumps, often occur with an allergic reaction or sometimes a viral infection. Or sometimes, they can be more serious when they happen with a severe allergic reaction called anaphylaxis.
Most of the time, you can find what caused them. But what if you cant?
There is a condition called chronic idiopathic urticaria (ur-ti-KAIR-ee-uh). Simply put, it means hives that stick around for more than six weeks for no known reason. Many people call it CIU. About 1.5 million people in the U.S. have it.
What Is CIU?
Hives caused by an allergic reaction or a viral infection usually go away after a short time.
CIU is different. It can be harder to diagnose. Women are more likely to have CIU than men. Symptoms usually occur between the ages of 20 and 40. For many, the condition typically lasts 1 to 5 years.
Some signs of CIU are:
- Itchy red bumps (hives) anywhere on the body
- Hives that last longer than 6 weeks (maybe even months or years)
- Hives brought on by no known cause
- Unpredictable symptoms that come and go
- Isnt always relieved by allergy medicines
No one really knows what causes CIU. They do know that heat, cold, alcohol, exercise, tight clothes and nonsteroidal anti-inflammatory medicines (ibuprofen, aspirin) may make it worse.
CIU is not life threatening. But sudden hives can be one of the symptoms of a severe allergic reaction.
Go to the emergency room or call 911 if:
- Your hives are severe and cover a large area of your body
- You have other symptoms such as difficulty breathing
What Do I Do If I Think I Have CIU?
If you think you have CIU, see a board-certified allergist or dermatologist. Both types of specialists treat CIU. They will do a physical exam and ask about your medical history. They may also do allergy testing and blood tests, if necessary.
How Is CIU Treated?
Your doctor may try a combination of different medicines to try to relieve CIU. They may first prescribe an allergy medicine called an antihistamine.1 If that doesnt work, there are other medicines your doctor may try until they find the ones that work for you.
Treatment may lessen your symptoms but not relieve them completely. Since CIU can be frustrating, support may help you cope as well. Support groups, such as the Asthma and Allergy Foundation of Americas Skin Conditions Support forum, can connect you with others with CIU. Talking to others who understand what youre going through can be comforting.
Medical Review September 2017.
It is important to stay up-to-date on news about asthma and allergies. By joining our community and following our blog, you will receive news about research and treatments. Our community also provides an opportunity to connect with other patients who manage these conditions for support.
References1. Godse, K. V. (2009). CHRONIC URTICARIA AND TREATMENT OPTIONS. Indian Journal of Dermatology, 54(4), 310312. http://doi.org/10.4103/0019-5154.57603
Hives (Urticaria)
What are hives?
Hives, or urticaria, are flat red welts that can appear anywhere on the skin and usually itch. Hives often occur as an allergic reaction to something eaten or something that has contacted the skin. Foods, medicines, and plants are common causes, but sun exposure, stress, infections, and autoimmune diseases have also been known to cause hives.
Symptoms include an itchy, stinging pink rash of slightly swollen skin. The rash may wax and wane in severity. Acute hives typically resolve within six weeks, but chronic hives (urticaria) can persist for months or years.
Hives often resolve on their own, especially in children. Otherwise, treatment for acute hives involves oral antihistamine medications to help relieve the itching and stinging. Chronic hives that do not improve with antihistamines may be treated additionally with corticosteroids, antibiotics, and other stronger medicines. A study found that 35% of people with chronic hives, are symptom free within one year, with another 29% having some reduction of symptoms.
You can safely treat this condition on your own as long as you does not develop trouble breathing. Any antihistamine (like Zyrtec, Clarinex, etc) works.
What to Do When Antihistamines Arent Working for Hives
Antihistamines may not work for some people, depending on the severity of their hives. You may need an increased dosage or a different medication altogether.
After a chronic idiopathic urticaria (CIU) diagnosis, your doctor will likely prescribe an oral antihistamine to treat your symptoms. However, antihistamines arent always effective.
If youve already tried an antihistamine and you arent seeing results, schedule an appointment with your doctor to learn about possible next steps.
Here are some questions you can ask your doctor at your follow-up appointment and some information about what you might hear in response.
Its hard to say why antihistamines work for some people and not for others. But its not uncommon for antihistamines to be or become ineffective.
Research on the effectiveness of antihistamines for chronic hives has shown a response rate as low as
Antihistamines may stop working because hives can become worse over time or because the intensity of hives can wax and wane over time.
Its also possible that antihistamines become less effective because people arent taking them as prescribed.
Even if you cant identify the cause of your CIU, you may be able to pinpoint triggers that bring on outbreaks or increase the severity of your hives.
See whether any of the following common triggers seem to affect you:
- pets or pet dander
- exposure to extreme heat or cold
- exposure to direct sunlight
- vigorous exercise
- pressure on the skin
- stress or anxiety
- nonsteroidal anti-inflammatory drugs (like ibuprofen)
By understanding your personal triggers, you can put yourself in a better position to avoid them.
After seeing little to no results from an antihistamine, your doctor may suggest that you try the following treatments, usually in the following order:
- Higher dose: Sometimes increasing the dose of your current antihistamine can yield better results.
- A different antihistamine or a combination of several different antihistamines. Your doctor may consider switching you to a different antihistamine or putting you on a regimen of two types of antihistamines. For example, they may recommend an H1-antihistamine combined with an H2-antihistamine, which targets different receptors in the body.
- Oral corticosteroids. While doctors usually dont recommend prolonged use of steroids due to potential side effects, they may recommend a short course. This is especially likely if your hives are severe or if theyre accompanied by swelling.
- Cyclosporine (Gengraf, Neoral, Sandimmune): This is an immunosuppressant drug that has led to remission from hives in
50% of cases , according to research. - Omalizumab (Xolair). Your doctor may recommend omalizumab, a medication thats injected once a month if your hives are difficult to treat, but is effective in 80% of cases.
- Leukotriene receptor antagonists (LTRAs): Two drugs, zafirlukast (Accolate) and montelukast, might be prescribed in cases of hives caused by Aspirin, and there isnt enough data on their effectiveness on hives overall.
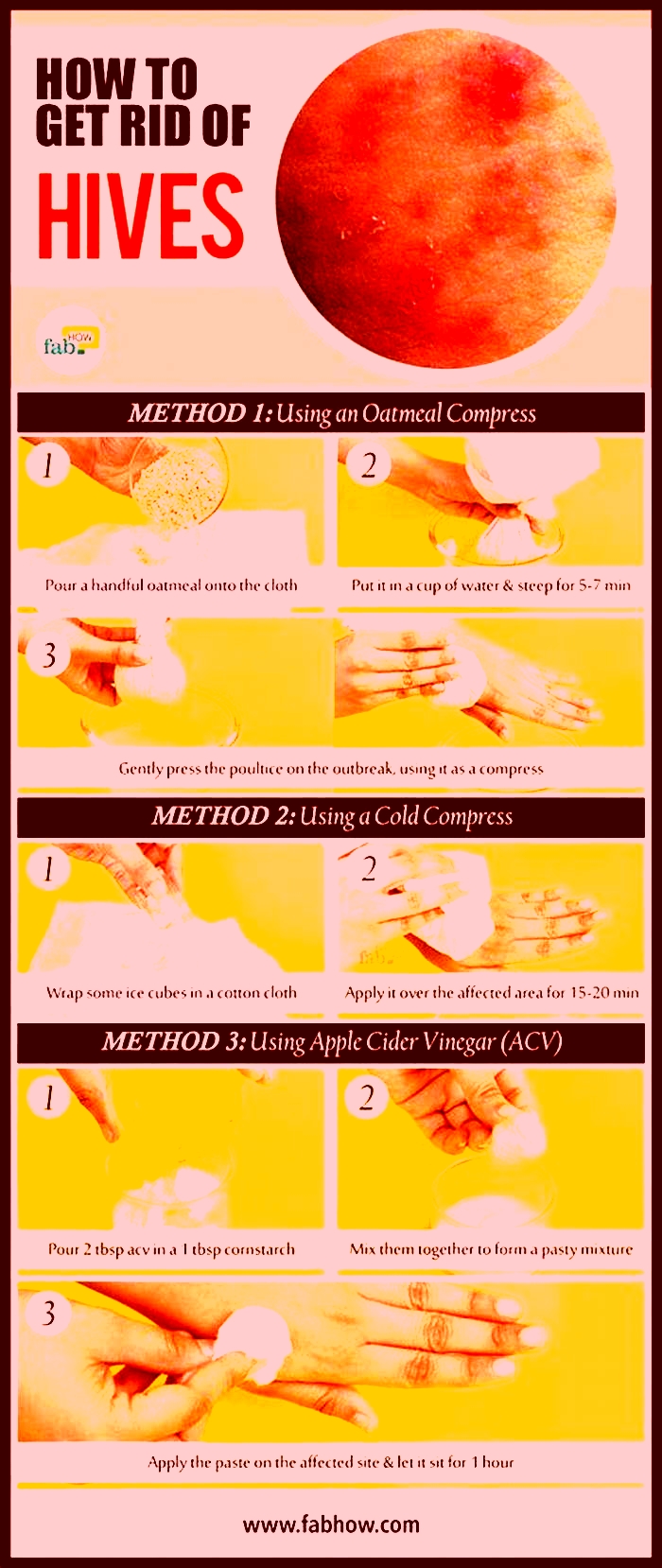
If your medication isnt giving you the relief you need, you can try the following methods to ease itching:
- Moisturize regularly with lotion.
- Use cool water when you shower.
- Apply a cold compress or an ice pack to affected areas.
- Try using over-the-counter creams such as calamine lotion.
- Wear loose clothing made from 100% cotton or 100% silk.
While none of the above methods will treat your CIU, they can at least provide comfort during a flare-up.
Dietary changes to help prevent hives
Researchers are still studying whether changing your diet can impact the severity and duration of CIU flare-ups.
A 2018 preliminary Korean study suggests that an antihistamine diet, where you avoid foods that contain high levels of histamine, may help reduce the severity on an individual level.
Since this and other similar studies only involved a small group of participants, researchers arent ready to draw wide conclusions about the diets success rate.
Even so, it may be worth talking with your doctor to see whether changing your diet is a good option.
No. Hives are never contagious, so you dont need to worry about spreading them to friends, family members, or others who are in close contact.
You also dont have to worry about the hives spreading if you touch other parts of your body after touching your hives.
If youre concerned about what other people will think when they see the welts on your skin, you can ask your doctor to provide a note explaining the nature of CIU and its symptoms. This can be especially useful for school-aged children.
No. While it may be frustrating to learn that antihistamines arent effective at treating your hives, you dont need to worry that they will leave any permanent marks or scars.
Most hives last for no longer than 24 hours and should fade and disappear after that.
While most cases of CIU arent dangerous, there are several warning signs that you should be aware of. Sudden and severe hives can mean youre experiencing an allergic reaction and need urgent medical attention.
If you experience any of the symptoms of anaphylaxis alongside a hives outbreak, call 911 or go to the emergency room:
By definition, chronic means that your hives will last for 6 weeks or more. But theres no way to say for sure exactly how long a specific outbreak episode will last. It could be months or even years.
Each individual welt will probably last for several hours, but theyre often quickly replaced by new ones.
The good news is that CIU can go away, its just hard to predict when.
Should I see an allergist?
If youve already been diagnosed with CIU, your doctor believes the cause is unknown and an allergy isnt to blame. But if you suspect that your doctor overlooked an underlying allergy, you may want to consider seeing an allergist.
What happens if hives dont go away with Benadryl?
Benadryl (diphenhydramine) is an over-the-counter antihistamine that can be used to treat mild allergic reactions, including hives. It is an H1 antihistamine, which means it is one of the ones your doctor may want you to try first. It is also available in higher doses as a prescription if the OTC version doesnt work for you. If its still ineffective, your doctor will likely switch you to H2 antihistamines, other medications, or a combination of drugs.
Why is Benadryl not stopping my allergic reaction?
If there is an ongoing trigger for your hives in your environment, you might continue to develop them or they may worsen even if youre taking an antihistamine like Benadryl. In addition to taking medication, its important to try to identify the trigger and eliminate it. To do this, make an appointment with a dermatologist or allergist for testing, and track your flare-ups. That said, sometimes there is no identifiable cause. Make sure you are taking your medication exactly as prescribed or following the directions on the box of any OTC drug.
If antihistamines dont work for you, dont become discouraged. This happens for certain people and under certain circumstances.
Ask your doctor about possible next steps. Whether that involves a different form of medication or introducing some natural steps to reduce itching, you have options to decrease CIU-related discomfort.
Mayo Clinic Q and A: Chronic Hives Come and Go With No Clear Pattern
Featured News
Mayo Clinic Q and A: Chronic Hives Come and Go With No Clear Pattern
 DEAR MAYO CLINIC: I woke up this morning with itchy, red welts covering my arms and legs. These have shown up every now and then over the past few months, and now they seem worse than usual. What could be causing this? How is it treated?
DEAR MAYO CLINIC: I woke up this morning with itchy, red welts covering my arms and legs. These have shown up every now and then over the past few months, and now they seem worse than usual. What could be causing this? How is it treated?
ANSWER: What you may be experiencing is chronic hives. Hives (urticaria) are raised, red or white itchy welts on your skin. A sudden onset of hives (acute hives) usually has an identifiable cause or trigger such as insect stings or bites, medications, certain foods, allergens, or infections. Acute hives go away within a few weeks and are usually effectively treated with antihistamines.
Chronic hives are different in that they persist for more than six weeks. The hives seem to come and go with no clear pattern fading over the course of a day or two and then reappearing in a different location a few days later.
Anyone can develop chronic hives, but theyre more common in middle-aged women. Chronic hives can go on for months and even years. They can interfere with sleep, work and other activities. Itching can be severe and may be accompanied by painful swelling. Signs and symptoms tend to flare up with heat, exercise or stress.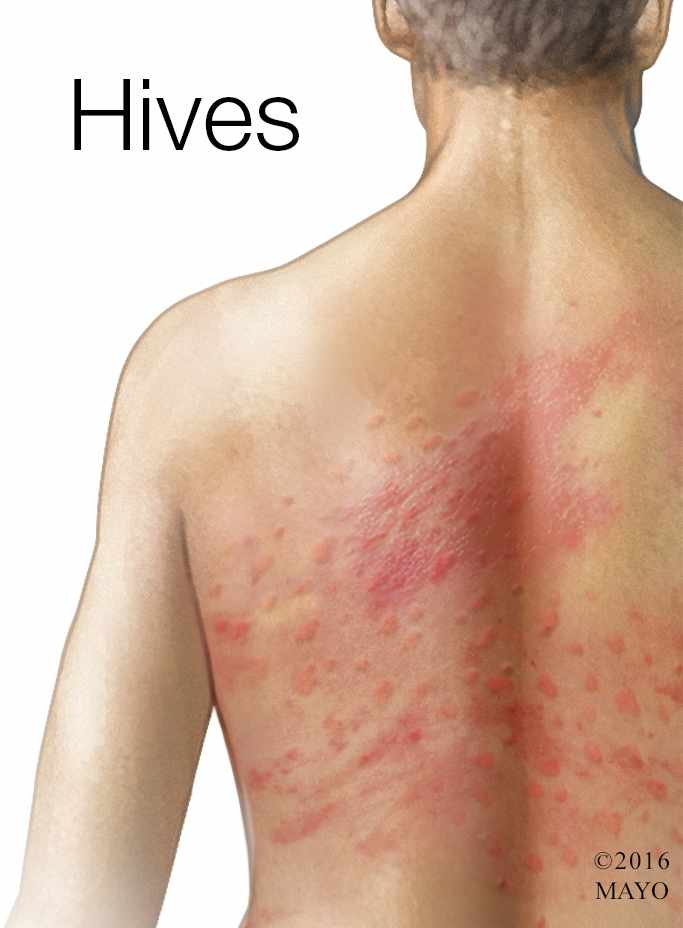
One of the biggest sources of frustration with chronic hives is wondering whats causing them. The truth is that its hard to know. Up to 90 percent of cases remain unexplained no external factor or contributing disease can be pinpointed as the cause.
People with chronic hives often are anxious that the hives may be a sign of a serious problem. While its possible for chronic hives to be associated with an underlying illness, such as an infection, autoimmune disorder or certain cancers, this is pretty rare.
A sudden onset of hives can be part of a serious allergic reaction (anaphylaxis). Signs and symptoms may also include swelling of your tongue or throat, breathing problems, and vomiting. And while anaphylaxis requires emergency care, chronic hives dont put you at any sudden risk.
To make an accurate diagnosis, your doctor will want to examine your hives. This may mean seeing your doctor when the hives show up. Your doctor also will want to know how often they appear, how long they last, whether you have any painful swelling, and if you have any other signs and symptoms, such as fever, unintentional weight loss, sensitivity to cold or heat, or pain in your abdomen, bones or joints. If your physical exam and medical history suggest there might be an underlying problem causing the hives, your doctor may recommend additional testing, such as blood tests or skin tests.
If the pattern of your symptoms is consistent with chronic hives, your doctor will want to know if youve started any new medications, traveled recently, or had any infections or other illnesses that might be contributing to the hives.
Providing your hives arent complicated by any additional signs and symptoms, and they cant be explained by any recent changes in your life, your doctor may recommend starting treatment with an over-the-counter nondrowsy antihistamine every day. Common examples include loratadine (Claritin, Alavert), fexofenadine (Allegra) or cetirizine (Zyrtec). If this doesnt work for you, be sure to tell your doctor. He or she may increase your dose or try a different kind of antihistamine. Medications such as corticosteroids or histamine (H2) blockers also are possibilities. If antihistamines dont control the hives, your doctor may prescribe treatment with omalizumab (Xolair), an injectable medicine thats usually given once a month. In most cases, an effective treatment can be found.
Evidence suggests that certain factors such as heat, tight clothing and nonsteroidal anti-inflammatory drugs (NSAIDs) can worsen chronic hives. Try to keep cool, avoid hot showers, and wear loose, comfortable clothing. If you take NSAIDs regularly for pain relief, talk to your doctor about switching to a different form of pain reliever, at least while you continue to have hives.
People often wonder if something in their diets might be causing their hives. Theres very little evidence that certain foods or food additives are responsible for chronic hives. But you may want to keep a food journal alongside a record of your symptoms so that you can detect a pattern, if any. Most doctors dont recommend any specific diet or dietary elimination.
Although you may never know the cause of your hives, you can rest assured that chronic hives are often temporary. Investigators followed more than 200 people with chronic hives for up to five years. They found that about half the people with unexplained chronic hives were free of symptoms within a year. In the majority of cases, chronic hives can be successfully controlled with medications and possibly a few lifestyle changes. (adapted from Mayo Clinic Health Letter) Dr. James Li, Allergic Diseases, Rochester, Minn.