Why do hives get worse at night
Can COVID-19 Cause Hives at Night?
Hives are a common symptom of COVID-19 that can occur during the day or night. Hives only at night might be from something youre coming into contact with in the evenings.
COVID-19 can cause hives during the day and night. They often show up early in the infection and may even be the first symptom you notice.
COVID-19 can cause several skin symptoms, including rashes and hives. These symptoms are typically brief, but in some cases, they last for months after the initial infection.
Hives develop when your immune system releases histamine in response to a perceived threat, like an allergen or infection. While hives can occur with infections like COVID-19, theyre more often associated with allergic reactions. You can have an allergy to something you eat, a medication youre taking, or an irritant that touches your skin.
Keep reading to learn more about hives and their connection to COVID-19, and whether its normal for them to appear only at night. Also, learn about treatments for hives and other skin conditions triggered by COVID-19.
Research has identified a link between hives and COVID-19. According to a
Researchers examined 63 articles and discovered that hives usually appear with other COVID-19 symptoms, like cough and fever. They last an average of 6.8 days.
Medications used to treat COVID-19 can also trigger hives.
Doctors need to conduct more research into how the coronavirus triggers hives.
Researchers in a 2020 literature review analyzed 46 articles that pooled the details of 998 people who got COVID-19 early in the pandemic. Among this group, 89 people, or 8.9%, developed hives.
Researchers noted that skin conditions are underreported with COVID-19 because they may develop early in the infection before other more identifiable symptoms appear.
Its normal for hives to come and go. But hives that appear only at night arent a symptom typically associated with COVID-19.
If youre getting hives only at night, it may be because youre coming into contact with an allergen in the evenings.
Detergents in clothes or bedsheets, lotions, or medications you take before bed could all cause hives at night. Alpha-gal syndrome can also trigger hives at night.
Alpha-gal syndrome is caused by a tick bite. The condition can cause hives or an itchy rash after eating meat or other animal products.
These hives take
Possible causes of hives at night
If you get hives only at night, it may be related to something youre coming into contact with late in the day. Some possibilities include:
- detergents used on clothing or sheets
- lotions or creams applied at night
- medication taken at night
- stress
- pressure from tight clothing, like a belt, or any part of the body under continual pressure
- changes in temperature, like very cold air or water, sweating, or a hot shower
- environmental allergens, like dust, mold, pollen, or animal dander
There are several ways that COVID-19 can affect your skin.
The
Other rashes that might appear when you have COVID-19 include:
Maculopapular
A maculopather rash is an itchy rash with both flat and raised parts. It often appears on the torso but can develop anywhere on the body. It can appear before or after other COVID-19 symptoms and typically lasts about 812 days.
Chilblain-like
Commonly known as COVID toes, this chilblain-like condition causes swelling and redness in your toes and, less commonly, your fingers. Its more common in children and young adults. It usually appears later in the infection.
Vesicular
A vesicular type of rash causes a blister-like appearance. Its more common in middle-aged adults. It may appear 430 days after other symptoms, with an average onset of 14 days. Typically, the rash clears up within 810 days.
Petechiae
Petechise is a rash that produces small, pinpoint red, purple, or brown spots beneath the skin on the torso, arms, and legs. Its not as common with COVID-19 as other rashes, but it can appear after other symptoms.
Livedoid eruptions
This rare symptom produces a blotchy rash that looks like a net. It appears at the same time as other symptoms. On average, it lasts about 9 days.
Hives can be distressing and itchy, but home remedies may help relieve discomfort. Most hives will go away on their own within a few hours, but while theyre visible you can:
- use an over-the-counter anti-itch cream, like calamine lotion
- apply a cold compress, like ice cubes wrapped in a towel, on areas that itch
- take an antihistamine or allergy medication
- use a fragrance-free moisturizer throughout the day
- practice self-care and stress-relieving strategies, as stress can trigger hives or make them worse
- keep a record of flare-ups to try and track the cause
- wear loose, breathable clothing
Many people experience an occasional outbreak of hives that respond to treatment at home.
If your hives last longer than 6 weeks or repeatedly flare up over this time, you may want to talk with a doctor. The American Academy of Dermatology recommends visiting a board certified dermatologist, allergist, or primary care doctor.
A doctor can help determine whats causing your hives and make sure nothing serious is going on. If they cant narrow in on the cause of your hives, your doctor might recommend allergy testing.
COVID-19 can cause several skin reactions, including hives. They usually appear at the beginning of the infection, sometimes before other symptoms develop. Hives from COVID-19 may come and go at any time of the day or night.
Hives that happen only at night are more likely caused by foods or other allergens, like detergents, lotions, or soaps. Things in your environment, like dust, pollen, and pet dander, can also trigger hives.
Most hives respond to over-the-counter treatment, like anti-itch creams, antihistamines, or allergy medications.
Hives (Urticaria)
What are hives?
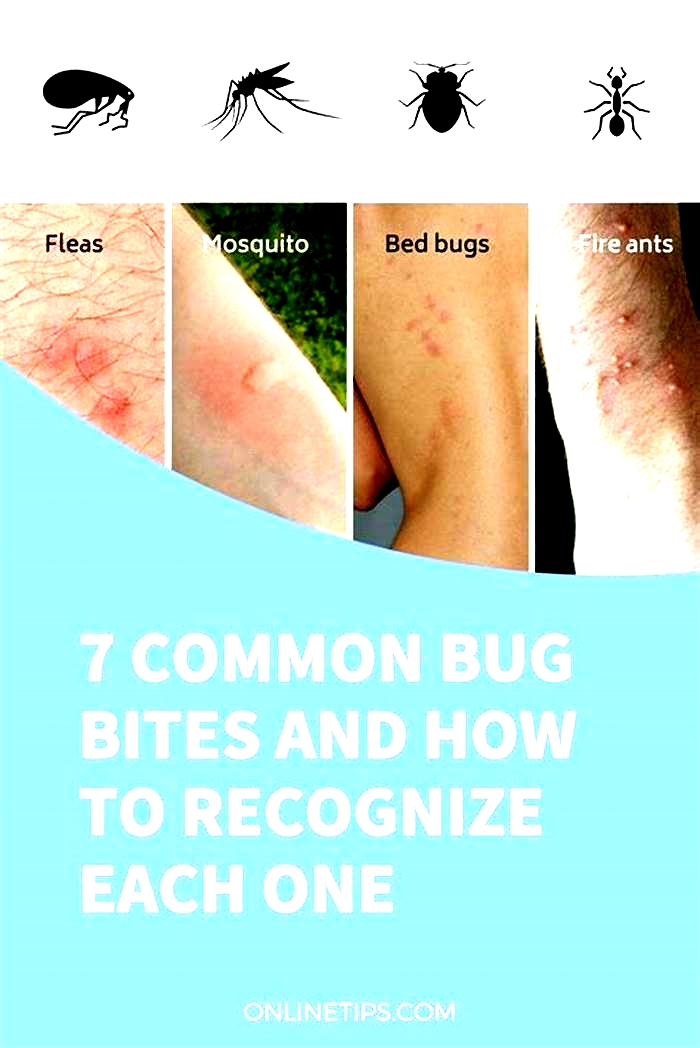
Hives, or urticaria, are flat red welts that can appear anywhere on the skin and usually itch. Hives often occur as an allergic reaction to something eaten or something that has contacted the skin. Foods, medicines, and plants are common causes, but sun exposure, stress, infections, and autoimmune diseases have also been known to cause hives.
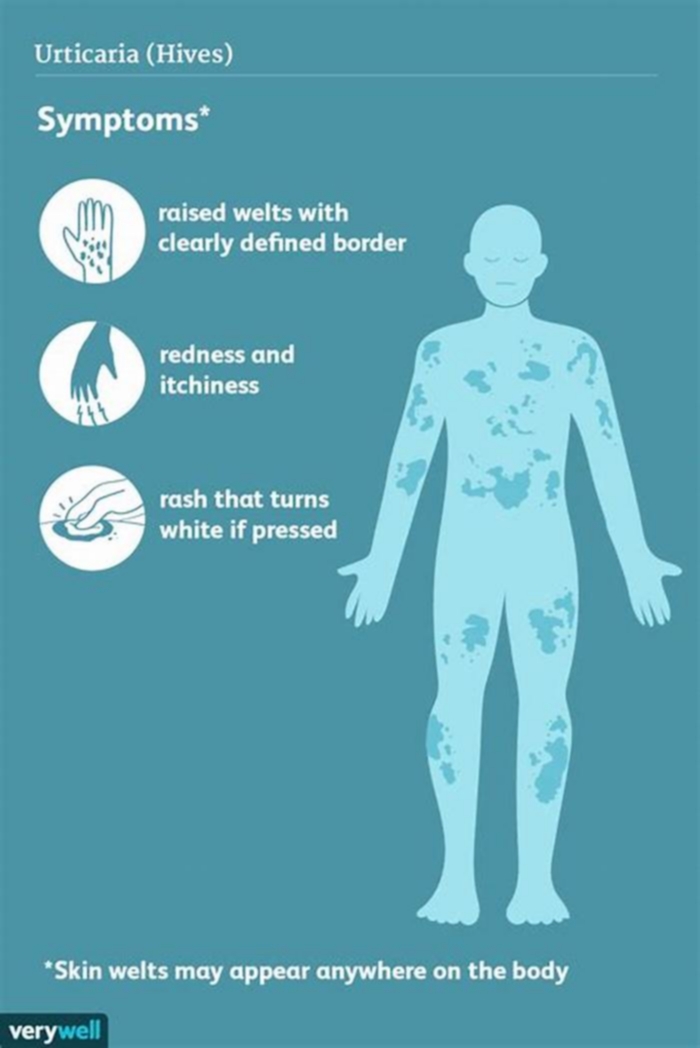
Symptoms include an itchy, stinging pink rash of slightly swollen skin. The rash may wax and wane in severity. Acute hives typically resolve within six weeks, but chronic hives (urticaria) can persist for months or years.
Hives often resolve on their own, especially in children. Otherwise, treatment for acute hives involves oral antihistamine medications to help relieve the itching and stinging. Chronic hives that do not improve with antihistamines may be treated additionally with corticosteroids, antibiotics, and other stronger medicines. A study found that 35% of people with chronic hives, are symptom free within one year, with another 29% having some reduction of symptoms.
You can safely treat this condition on your own as long as you does not develop trouble breathing. Any antihistamine (like Zyrtec, Clarinex, etc) works.
Hives at night: Alpha-gal syndrome?
For the past five nights, including tonight, I have been experiencing a reaction of some sort. I assume that they are hives. The weird thing is that it only happens, well 95% of the time, the breakout starts in the evening. I know it's not from a bite or something because they are in different spots each night... I have had an allergy test ..that was done a few years back and it came back negative. Not allergic to anything. I know that can change, but I just find it odd that this only happens at night. During the day, I am fine... just anxious know what's to come after sundown. Another thing I noticed is that they are usually in straight lines.. not always, sometimes they are blotchy but a lot of the time they are in lines. I have taken benadryl every night for the past few nights... didn't work. Tonight I got a little bit of relief but I can already feel my body getting itchy. Hydrocortisone creams do nothing. I think I just apply them for piece of mind. I called my primary's after hours answering service and spoke with my doc. I have an appt with her in the morning and she is going to do bloodwork and give me steroid shots, but I just wanted to see if anyone else has experienced anything like this before or know someone who has.
They usually last for the night. When I can finally get myself to sleep at night.. in the morning i am fine. They dont leave any markings or anything. They are just red and raised and extremely itchy.
Any input will help. Thanks in advance.
Interested in more discussions like this? Go to the Skin Health Support Group.
What causes hives that come and go daily?
Some people experience a flare-up of hives that goes away on its own. Other people may have hives that come and go daily.
Hives are itchy, raised bumps on the skin. Doctors diagnose chronic hives in people who experience them for at least 6 weeks. Each hive typically lasts for 24 hours before disappearing. Usually, the condition does not have an identifiable cause, but sometimes it does.
Some people experience chronic hives due to an underlying condition. Therefore, it is important for individuals to speak with a doctor about hives that keep returning.
Keep reading to learn more about the symptoms, causes, diagnosis, and treatment of hives that come and go daily.
Chronic hives is a condition that causes hives that keep coming back. Each one lasts less than 24 hours but, as old hives fade, new ones appear. If this continues for 6 weeks or longer, a doctor will diagnose chronic hives. Acute hives lasts less than 6 weeks.
The symptoms of both acute and chronic hives are the same. A person will have welts that come and go. In some cases, symptoms can hinder daily activities and impair sleep.
Chronic hives look identical to acute hives. In both cases, they can flare up and resolve, but chronic hives keep coming back for 6 weeks or longer and typically occur daily.
Hives are itchy, raised welts on the skin that may be red or the same color as a persons skin. Hives can develop anywhere on the body, move around, and change shape. They can also appear and disappear suddenly.
Hives usually do not break the skin, but bleeding can occur if a person scratches them.
Chronic hives can happen for various reasons. In most cases, however, it is not possible to identify the trigger.
Chronic idiopathic urticaria
The medical name for chronic hives that have no clear trigger is chronic idiopathic urticaria.
According to the American Osteopathic College of Dermatology (AOCD), the immune system is overactive in about half of people who have chronic idiopathic urticaria. Doctors consider these cases autoimmune, as they stem from the immune system attacking healthy tissues.
However, some
Bacterial infections associated with chronic hives include:
Viral infections associated with the condition include:
Parasitic infections associated with chronic hives include:
Autoimmune conditions
Some cases of chronic hives may stem from an underlying autoimmune disease.
Conditions associated with chronic hives include:
Research suggests that
Physical stimuli
Chronic hives can stem from physical stimulation, such as scratching or rubbing the skin. This is known as physical urticaria or dermatographism. The most common trigger is scratching or rubbing the skin firmly. The hives are not always itchy.
Other physical triggers may include:
- exercise
- cold temperatures
- hot temperatures
- sunlight
- vibration
- pressure
Allergies
As with acute hives, chronic hives can also occur due to an allergy. However, unlike acute hives, this is a
Some common allergens that can trigger hives include:
- certain foods
- food additives and preservatives
- latex
- medications
Reactions to medications can happen at any time after someone starts taking one. Some common triggers include:
Diagnosing chronic hives may begin with consulting a primary care physician, an allergist, or a dermatologist. They will examine the hives and ask the person questions to rule out common causes, such as a medication reaction.
A doctor may order diagnostic tests to check for other conditions that could be causing symptoms. This could include allergy testing, blood tests to detect inflammation markers, or tests for celiac disease or thyroid problems.
If the hives are not always apparent, it may help for a person to take photographs to show a doctor at the appointment. Keeping a diary of when the hives appear and any possible contributing factors may also help. People can track:
- food they eat
- medication they take
- exposure to physical stimuli, such as the sun, friction, or pressure on the skin
In cases where there is no clear cause, treatment focuses on managing the hives.
A doctor may recommend the
- Second-generation H1-antihistamines: This is the first-line treatment for chronic hives, and includes drugs such as cetirizine and loratadine. Routine use of first-generation H1 antihistamines, such as diphenhydramine (Benadryl), is not recommended by doctors due to sedating side effects.
- Omalizumab (Xolair): If symptoms do not respond to the first-line treatment, practitioners may add Xolair for a second-line treatment. It is a monoclonal antibody, which blocks the action of substances in the body that produce hives.
- Cyclosporine (Gengraf): Doctors may prescribe this when someone does not respond to a combination of an H1-antihistamine and omalizumab.
- Corticosteroids: Short-term use of these anti-inflammatory drugs may be an option to alleviate flare-ups of chronic hives. They are not suitable for long term use due to the risk of cataracts and other possible adverse effects.
If a person knows the trigger, avoiding it can help manage symptoms.
Chronic hives can go away. One study found that 35% of participants with chronic hives had no symptoms after 1 year, and another 29% experienced a reduction in symptoms during this time.
Among individuals with idiopathic chronic hives, 48% experienced remission within 3 years. However, only 16% of those with physical hives experienced remission within 3 years.
If a person has flare-ups of hives for 6 weeks or longer, the American Academy of Dermatology recommends visiting a board-certified allergist, dermatologist, or primary care doctor.
If someone experiences severe hives inside their mouth or airways that affect breathing, call 911 or the number of the nearest emergency department. This could be a sign of a severe allergic reaction, or anaphylaxis, which can make it hard to breathe and can be life threatening.
Here are some questions people often ask about chronic hives.
Why am I getting chronic hives?
In many cases, it is not clear what is causing hives. However, they may be linked to allergies and some immune conditions, such as lupus and celiac disease. Physical stimuli for instance, heat, pressure and vibration may also contribute.
Will chronic hives ever go away?
Chronic hives can go away over time, or symptoms may improve. However this does not happen for everyone. If hives go away, they can also come back in some cases.
How can I get rid of chronic hives?
It might not be possible to get rid of chronic hives, but treatment options such as antihistamines, corticosteroids, and other drugs can help manage symptoms.
Hives that come and go daily for at least 6 weeks are chronic hives. Most cases do not have an identifiable cause, but it is associated with an infection, autoimmune condition, allergy, or physical cause in some people.
Physical hives can occur due to exercise, vibration, or exposure to hot or cold temperatures. However, chronic idiopathic urticaria when there is no known cause is more common.
Chronic hives can affect a persons quality of life, but doctors can prescribe medications to help manage the symptoms.